 |
When Your Patient Complains of Headache
Learn what this signifies and what to do about it.
By Khadija Shahid, OD, MPH
Release Date: October 15, 2021
Expiration Date: October 15, 2024
Estimated Time to Complete Activity: 2 hours
Jointly provided by Postgraduate Institute for Medicine (PIM) and Review Education Group
Educational Objectives: After completing this activity, the participant should be better able to:
- Understand the etiologies behind headaches that present with an ophthalmic component.
- Ask the right questions when a patient complains of headaches.
- Understand how optometric services can mitigate complaints of headaches.
- Identify the more serious conditions that may present with a headache.
- Determine whether or not a referral to a specialist is needed.
Target Audience: This activity is intended for optometrists engaged in managing patients who present with headaches.
Accreditation Statement: In support of improving patient care, this activity has been planned and implemented by the Postgraduate Institute for Medicine and Review Education Group. Postgraduate Institute for Medicine is jointly accredited by the Accreditation Council for Continuing Medical Education, the Accreditation Council for Pharmacy Education, and the American Nurses Credentialing Center, to provide continuing education for the healthcare team. Postgraduate Institute for Medicine is accredited by COPE to provide continuing education to optometrists.
Reviewed by: Salus University, Elkins Park, PA
Faculty/Editorial Board: Khadija Shahid, OD, MPH
Credit Statement: This course is COPE approved for 2 hours of CE credit. Activity #122550 and course ID 74498-GO. Check with your local state licensing board to see if this counts toward your CE requirement for relicensure.
Disclosure Statements:
Author: Dr. Shahid has no financial interests to disclose.
Managers and Editorial Staff: The PIM planners and managers have nothing to disclose. The Review Education Group planners, managers and editorial staff have nothing to disclose.
 |
| Click table to enlarge. |
Headache, or cephalgia, is one of the most prevalent disorders in the world. Over half the population younger than 20 experiences headache at some point in their lives. By the time of adulthood, headache has occurred in over 90% of the total population, making it the most disabling neurologic disorder worldwide.1
The complex, subjective nature of cephalgia makes it challenging to manage, yet its pervasive and severe characteristics have led people to seek treatment as far back as the earliest documented time in human existence. Today, headache is still a common presenting complaint in the emergency department (ED) and the single most common neurologic complaint in pediatric ED visits.2,3
 |
| Fig. 1. Headaches are primary or secondary depending on the etiology. Click image to enlarge. |
Patients with headache are routinely referred to eye care physicians for consultation. Similarly, patients experiencing headache, or the associated visual and ocular symptoms, are more likely to present to us with questions and concerns. As optometrists, we needn’t feel the burden to act as a neurologist to our patient; rather, we should be familiar enough with the disorder to be part of the management team and triage appropriately when an emergent referral is indicated.
Headaches can be caused by something as simple as the wrong eyeglass prescription, or as urgent as a neuro-degenerative disorder. Determining which one is sitting in your chair might take some practice—and a thorough patient history.
This article will help clinicians understand the many etiologies behind a headache, not all of which require a referral to a neuro specialist. We will also discuss the more serious conditions that may give rise to headache and how clinicians can identify them early to ensure a quick referral when necessary.
 |
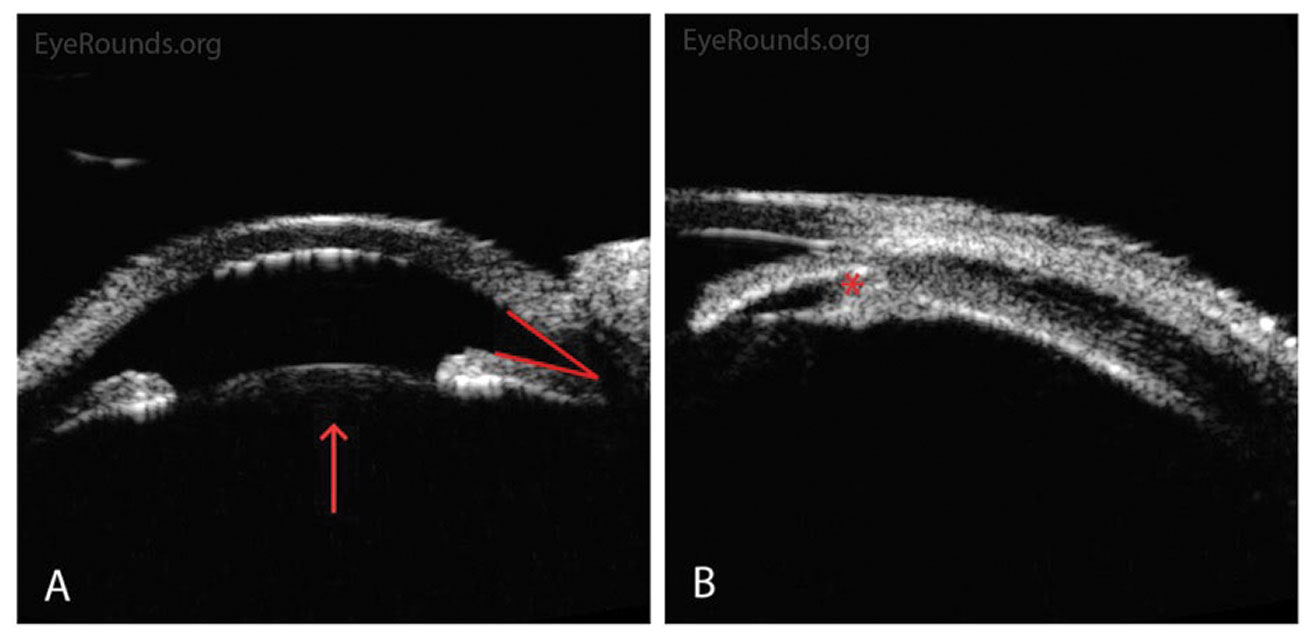
| Fig. 2. OCT of the optic nerve demonstrates mild retinal nerve fiber layer (RNFL) loss OD>OS and ganglion cell loss (GCL) loss OU. Click images to enlarge. |
 |
The OD’s Role
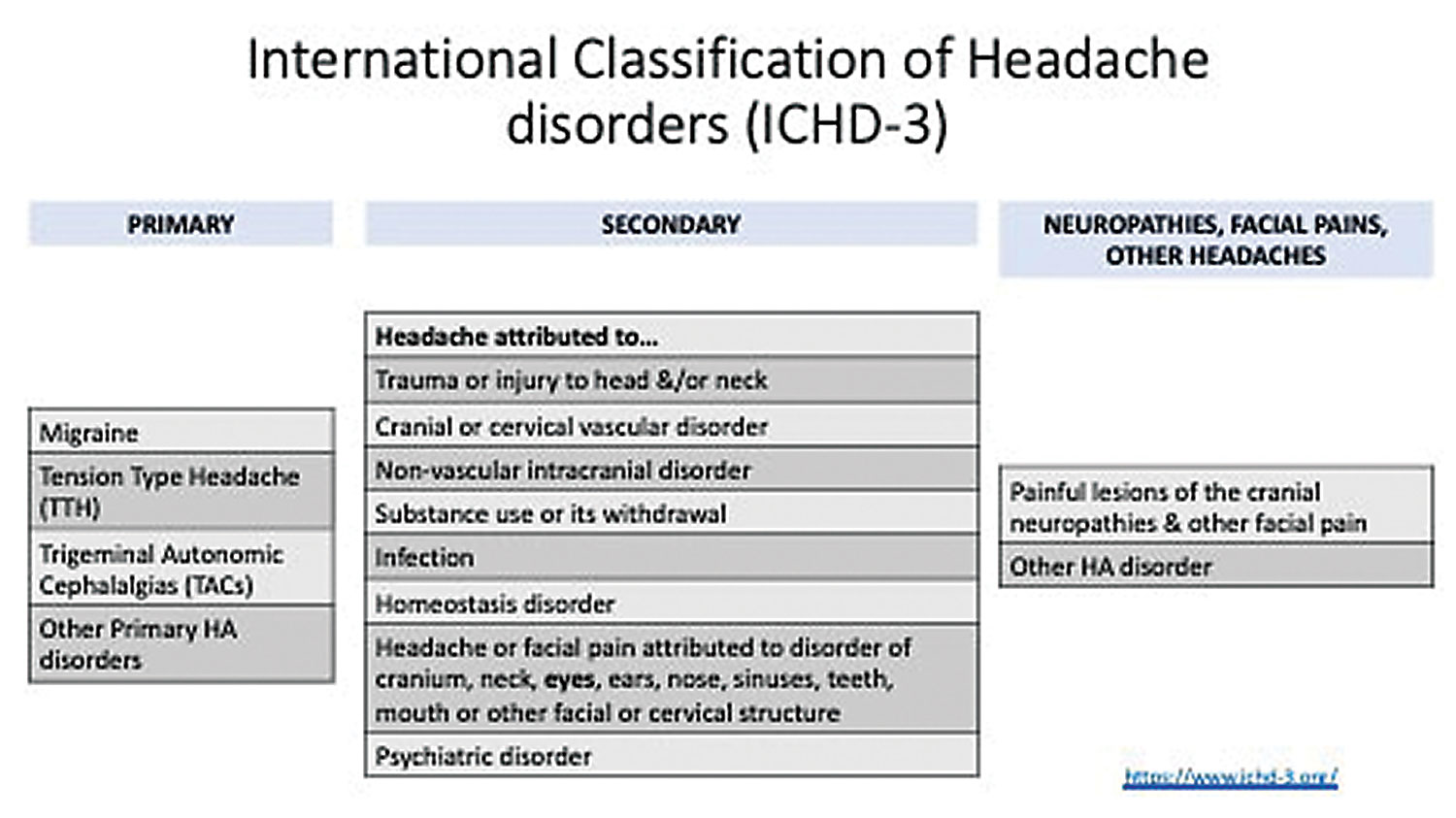
Headaches can be divided into primary and secondary types based on the underlying disorder, as outlined by the International Classification of Headache Disorders’ third edition (ICHD-3) (Figure 1).
Primary headaches are caused by dysfunction of pain-sensitive structures in the head. They comprise most headaches and include four major categories: migraine, tension-type headache, trigeminal autonomic cephalalgias (TAC) which include cluster headaches and other primary headache disorders.
The ICHD-3 defines secondary headaches as those related to underlying disorders such as trauma, infection, malignancy or uncorrected refractive error—the most relevant to eye care providers.
It’s important to consider the following in our role as optometrists when it comes to the headache workup:
Is the headache vision-related? Consider uncorrected or miscorrected refractive error, accommodative or binocular disorders, and computer vision syndrome. Patients will complain of frontal or temporal pain and asthenopia, worse during the work or school week and generally relieved by rest. Work, school and recreational screen viewing have increased exponentially, so even if the visual component isn’t the primary cause, it can be a significant contributor, warranting the need for best refractive correction and visual hygiene at all times.
 |
| Fig. 3. Goldmann VF testing demonstrates normal VFs with I2e and I4e isopter OU. Click image to enlarge. |
An important population to consider in this category are those suffering from traumatic brain injury. Over half of these patients report chronic headache along with increased dry eye and symptoms of fragile binocular systems, all of which can be addressed through optometric care.4
Does it originate in the eye? Consider corneal disorders such as dry eye, foreign body, abrasion, keratitis and herpetic eye disease, as well as angle closure and inflammation/uveitis. Headaches originating from the eye typically present as unilateral head pain or brow ache. Look for associated photophobia, decreased vision, nausea/vomiting and a red, painful eye.
Is it an emergent or urgent case? Look for concerning signs and symptoms such as intractable migraine (persistent, debilitating migraine lasting more than 72 hours, which is also referred to as status migrainosus), neurological changes including pupillary abnormalities and/or cranial nerve (CN) palsies, associated fever or infection and history of recent trauma. ODs should also watch out for cases of rapid-onset (arising and peaking within a few minutes) or “first-or-worst” headaches, especially in patients who are pregnant, immunocompromised or over the age of 50.
 |
| Click table to enlarge. |
Primary Headache
These types of headaches are the most common. As such, it is important that ODs recognize how to approach patients who present with them.
Migraines. This type of headache is the third most prevalent disorder in the world and the third leading cause of disability in people under the age of 50. The typical migraine sufferer is 25 to 55 years old and female (3:1 female-to-male ratio) with a family history of migraine.5
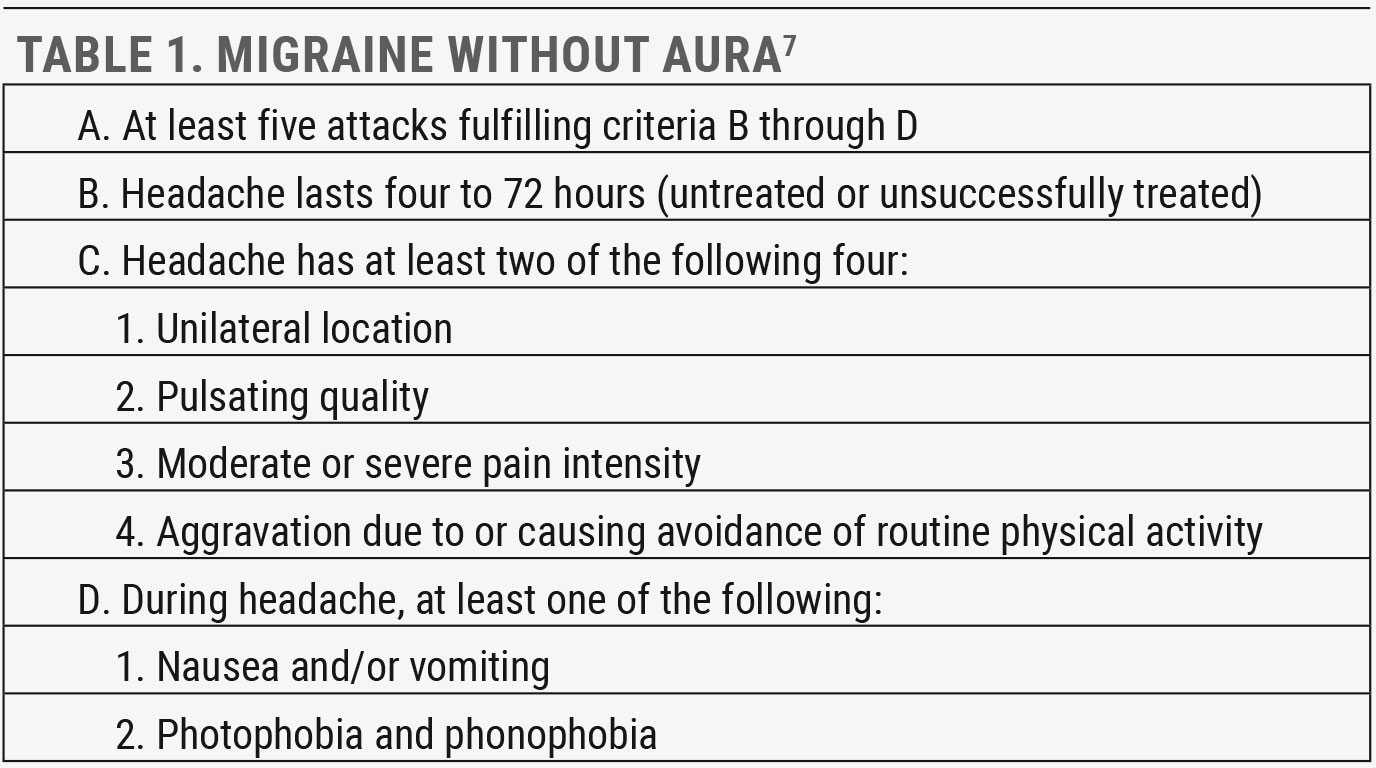
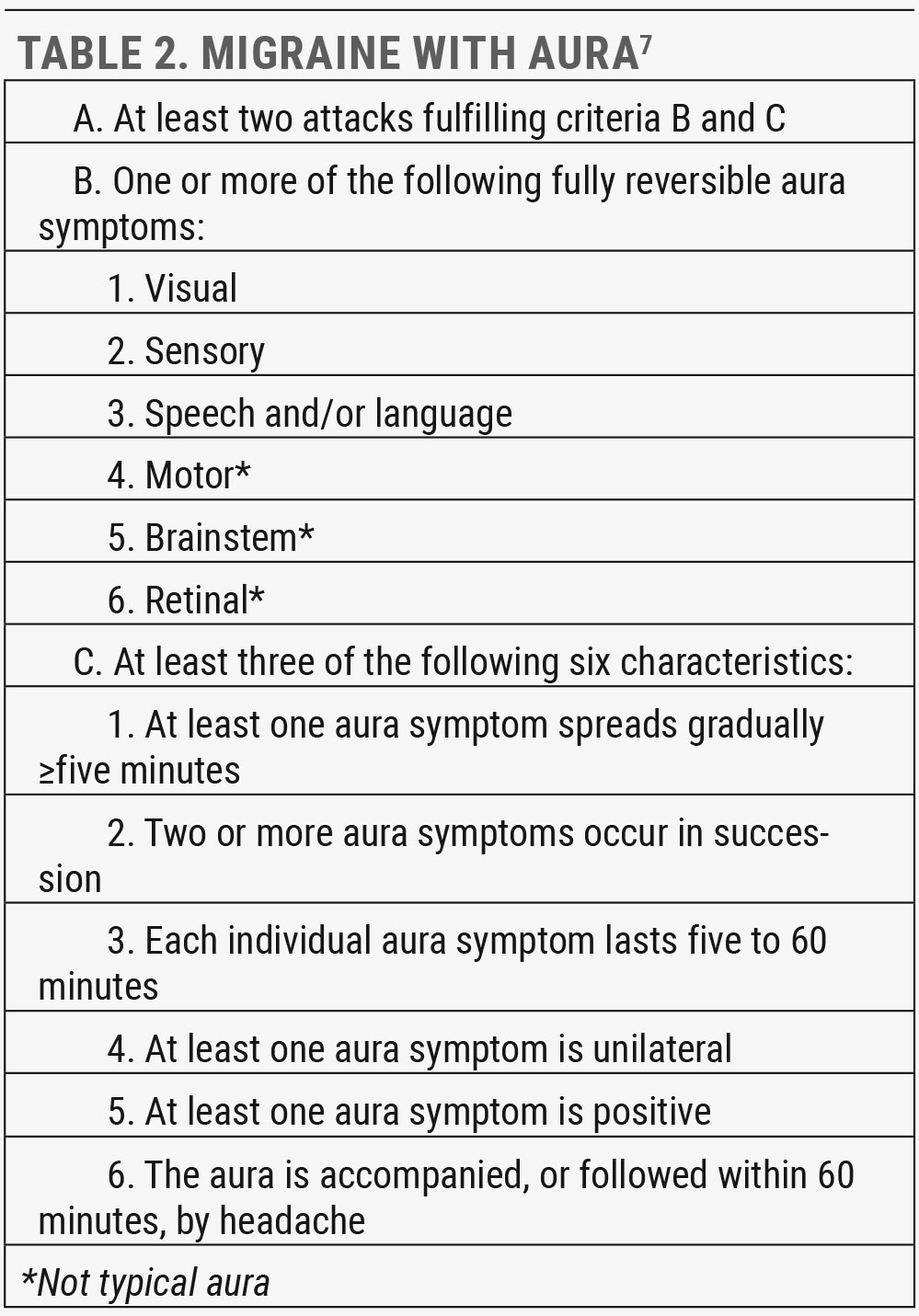
There are several types and subtypes of migraine outlined in ICHD-3, and many patients experience more than one over their lifetime. The most common is migraine without aura, occurring in over 60% of migraine sufferers, followed by migraine with aura, affecting approximately 30% (Tables 1 and 2).6
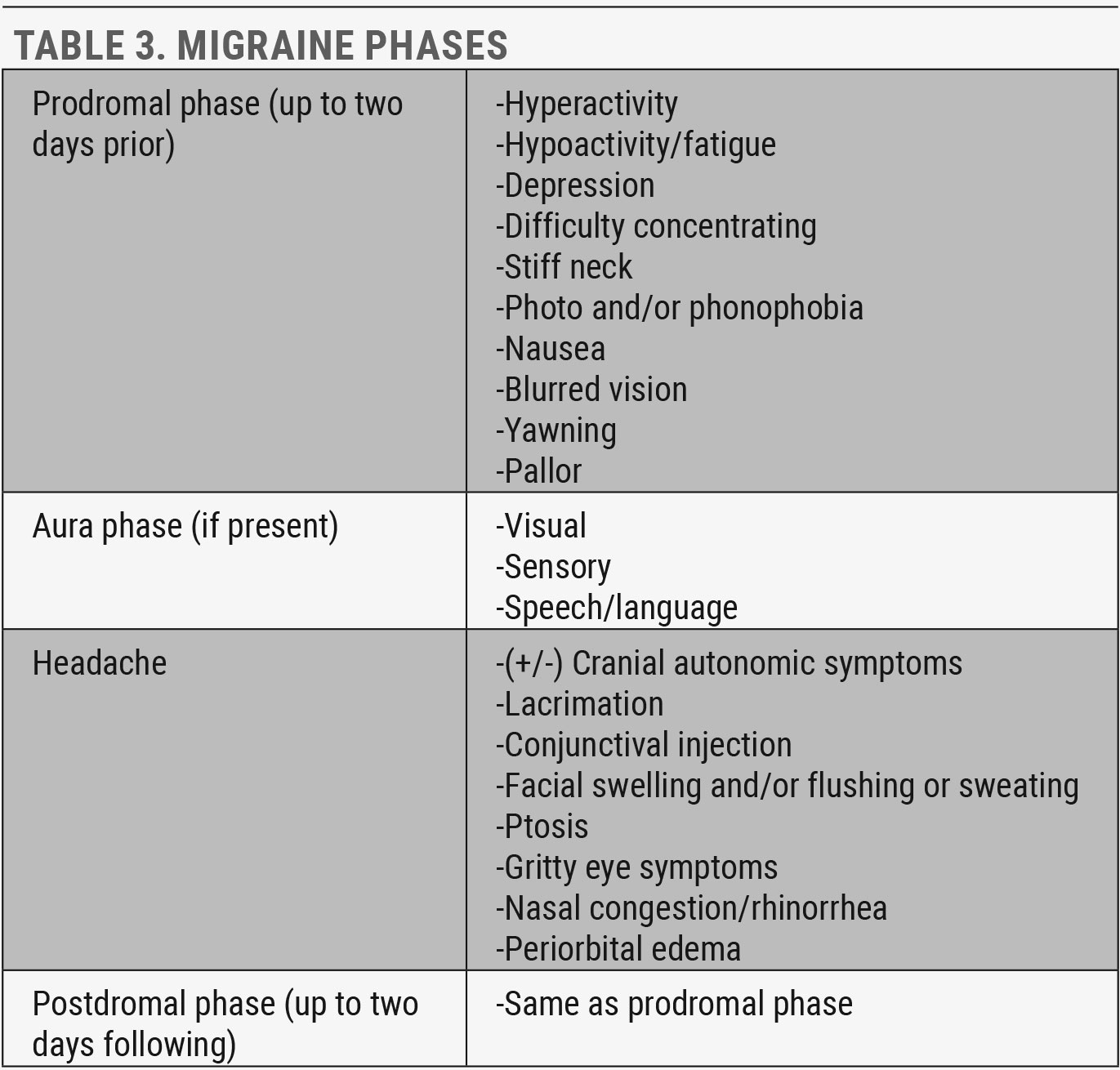
The typical migraine can occur in four phases which can begin up to two days prior to the headache attack and continue up to two days following (Table 3).
The aura phase is characterized by recurrent attacks of usually unilateral, fully reversible, visual, sensory or other central nervous system symptoms. These tend to develop gradually, persist for up to an hour and then fully resolve, although they can continue into the headache. More than one aura type can occur, generally in succession. The most frequent is visual aura, occurring in over 90% at least some of the time, followed by sensory (pins and needles) and speech aura (aphasia).7
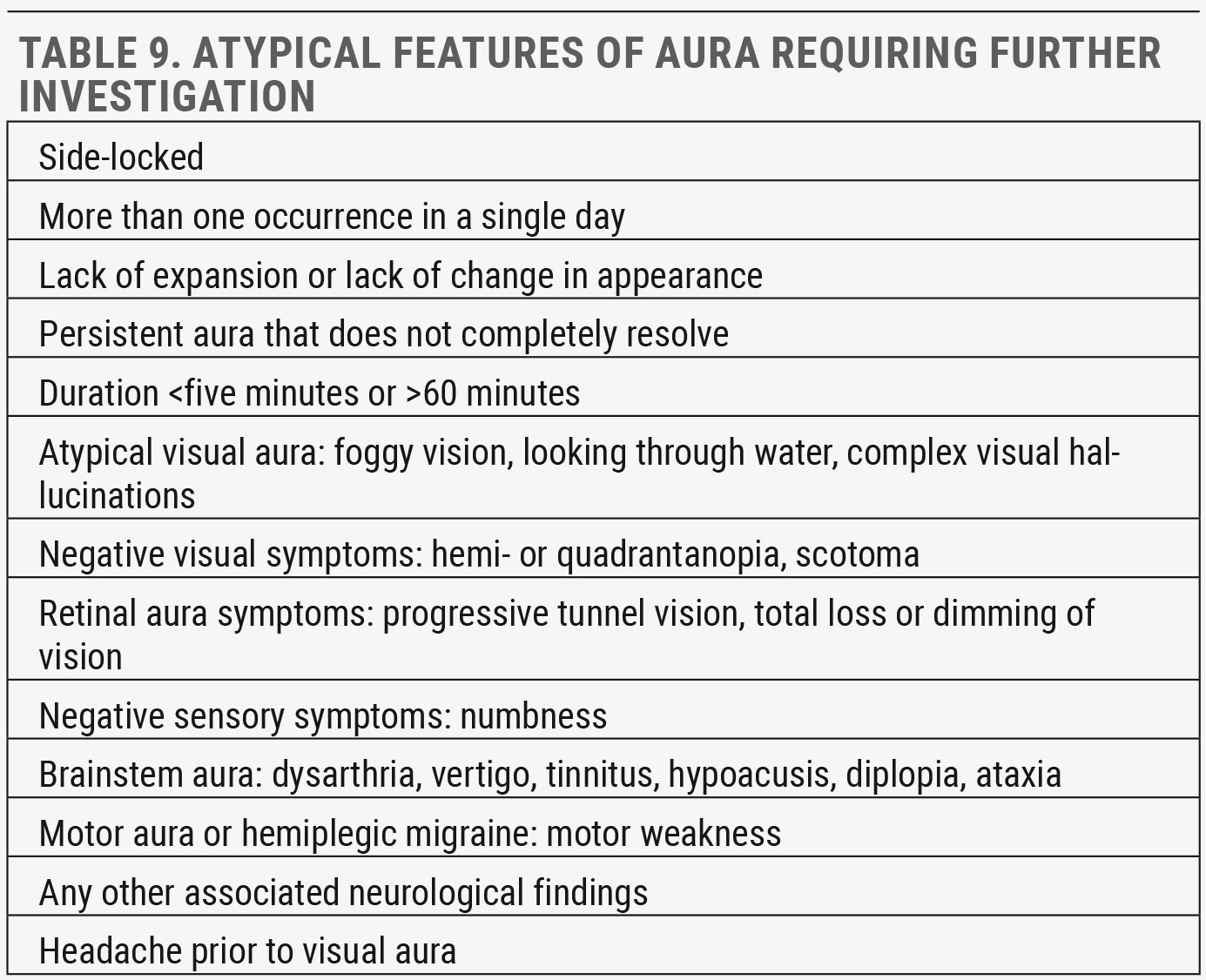
When atypical aura characteristics are described by patients or when rare complications of migraine present, a comprehensive eye exam and a prompt referral for additional neuroimaging or other workup is necessary to rule out infarction or other concerning differentials.
 |
| Click table to enlarge. |
Women have a unique relationship with migraine. They are at higher risk of migraine with more severity and frequency compared with men, in part due to hormonal correlations. Ten percent report more severe symptoms or increased attacks during menstruation, while 70% note improvement during pregnancy.8
There is an increased risk of stroke in males and females with chronic migraine, but especially in women with migraine aura and history of smoking. This risk may be further exacerbated by estrogen-containing oral contraceptives.9
As optometrists, we can counsel patients with chronic migraine to identify and minimize headache triggers and to maintain healthy lifestyles via optimal nutrition, hydration and weight, as well as adequate and regular sleep schedule and stress management (mindfulness practice, meditation, walking, etc.), all of which are proven to mitigate headache.10
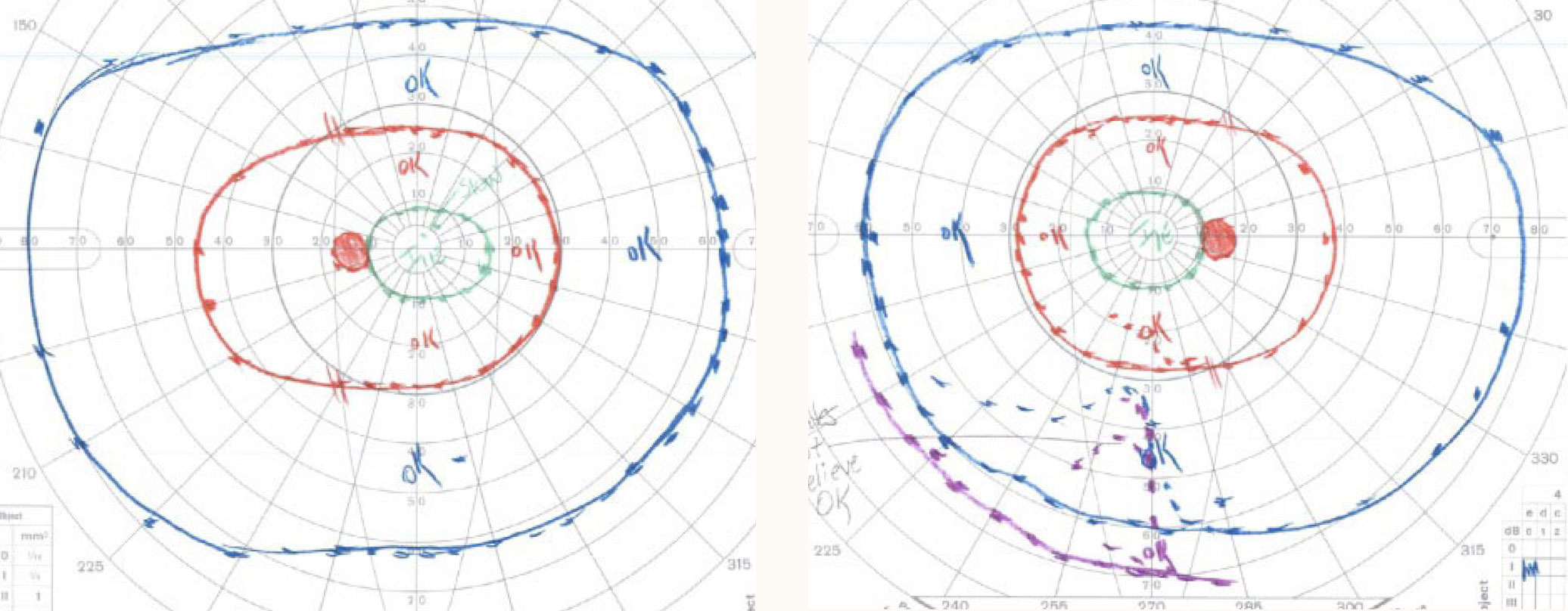
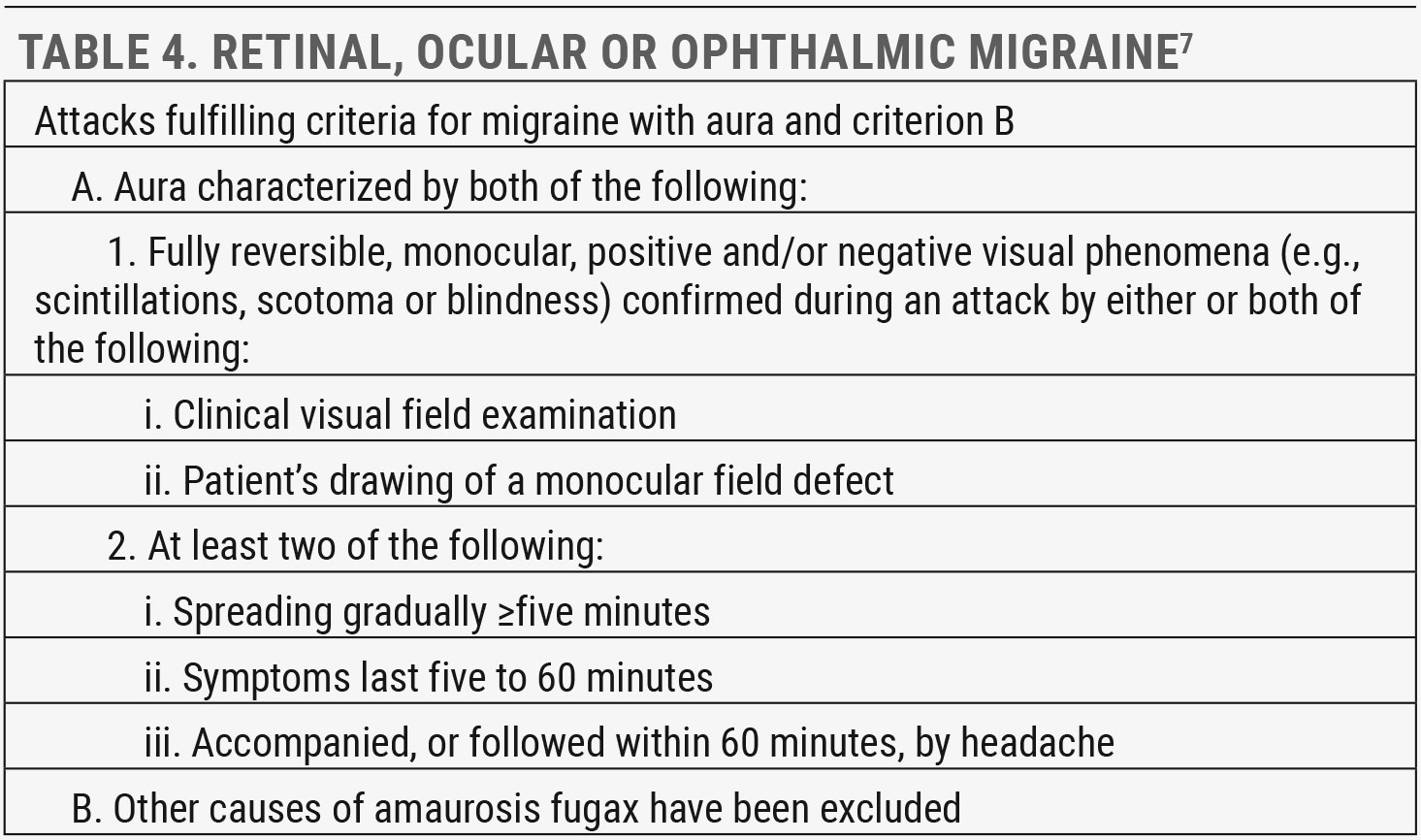
Retinal migraines. Much less common, but more likely to present to us, is retinal migraine. A retinal, ocular or ophthalmic migraine is a series of repeated attacks of unilateral visual disturbance (Table 4). The visual disturbance is always monocular, more commonly negative (dimming, scotomas or blindness) and often followed by ipsilateral headache. As this migraine type is very rare, the diagnosis is one of exclusion and can only be made after all other causes of transient monocular vision loss are ruled out.
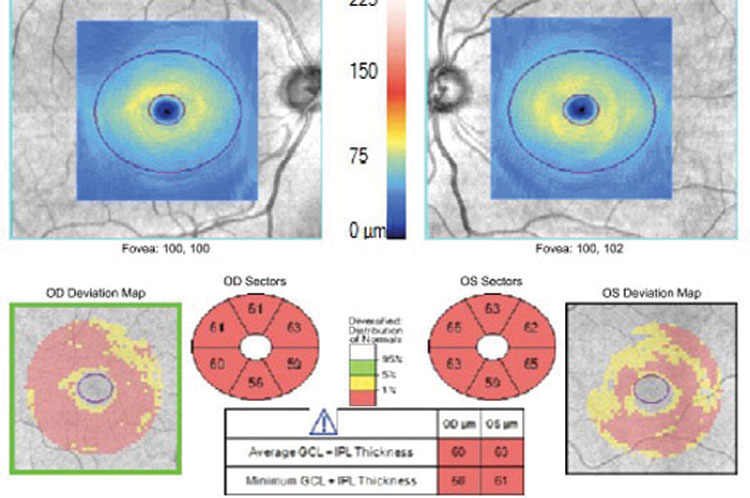
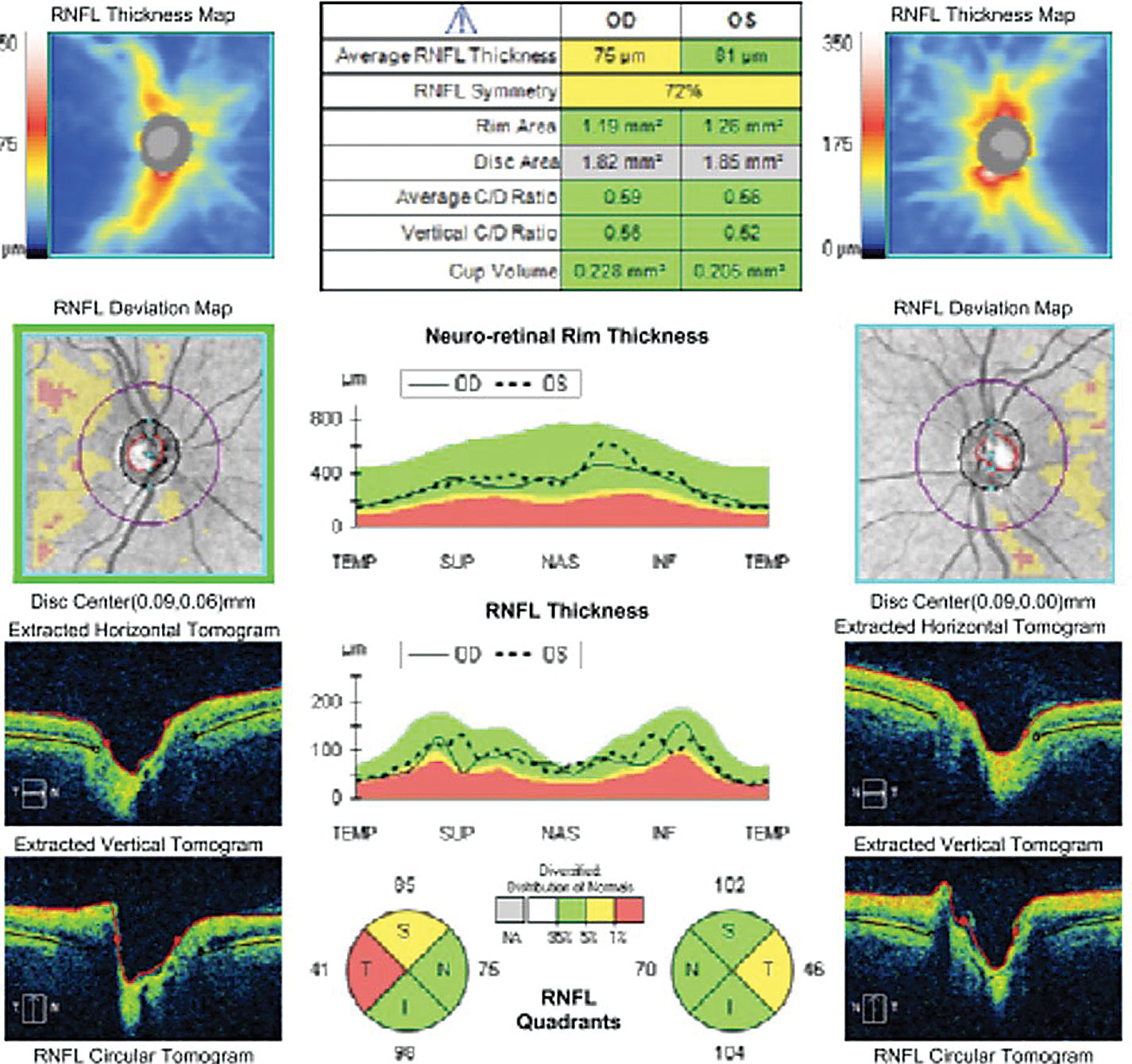
If you suspect your patient has experienced a retinal migraine, document important details of the history of present illness (HPI) and perform a thorough ophthalmic exam with particular attention to pupils, extraocular motility (EOM) and visual fields (VFs) through testing such as dynamic, Goldmann-type VF or static, Humphrey-type VF (Table 5).11 Record the aura either by having the patient draw the defect or via VF testing if the aura is present during examination.
 |
| Click table to enlarge. |
The posterior pole should be evaluated for optic nerve changes such as increased cupping (glaucoma), edema or pallor (demyelination, compression or ischemic optic neuropathy), presence of drusen (high suspicion for choroidal neovascular membrane or vascular occlusion) and a crowded disc (increased risk of vascular occlusion). Presence of macular edema and/or compromise of vascular arcades suggests central retinal artery or vein occlusion and/or other carotid artery disease or ischemia.
If the patient is experiencing a retinal migraine during the exam, you may note one or all of the following:12
- (+) RAPD during or after the attack
- (+) Benign episodic pupillary dilation, i.e., spontaneous pupil dilation for seconds, minutes or hours
 |
| Fig. 4. Anterior segment ultrasound shows a shallow anterior chamber, narrow angle, forward-displaced lens and anteriorly rotated ciliary body. Click image to enlarge. |
- Disc and macular pallor
- Vasoconstriction of arteriolar and venules (segmental or diffuse), which is the most common observation during an attack
Most importantly, even in the absence of ophthalmic or other findings, refer to the appropriate specialist for careful workup before making the diagnosis of retinal migraine. Direct communication should be initiated with the patient’s primary care provider (PCP), cardiologist or neurologist, with a suggestion to include the following in the workup: carotid testing such as carotid and cardiac auscultation, carotid Doppler study and cardiac echogram, as well as transesophageal echography and imaging of the brain, orbit and cerebral vasculature.
Patient/family history and additional symptoms may warrant further testing to rule out, for example, giant cell arteritis (GCA), collagen vascular disease, hypercoagulable states, vasculitis or obstructive sleep apnea (OSA),
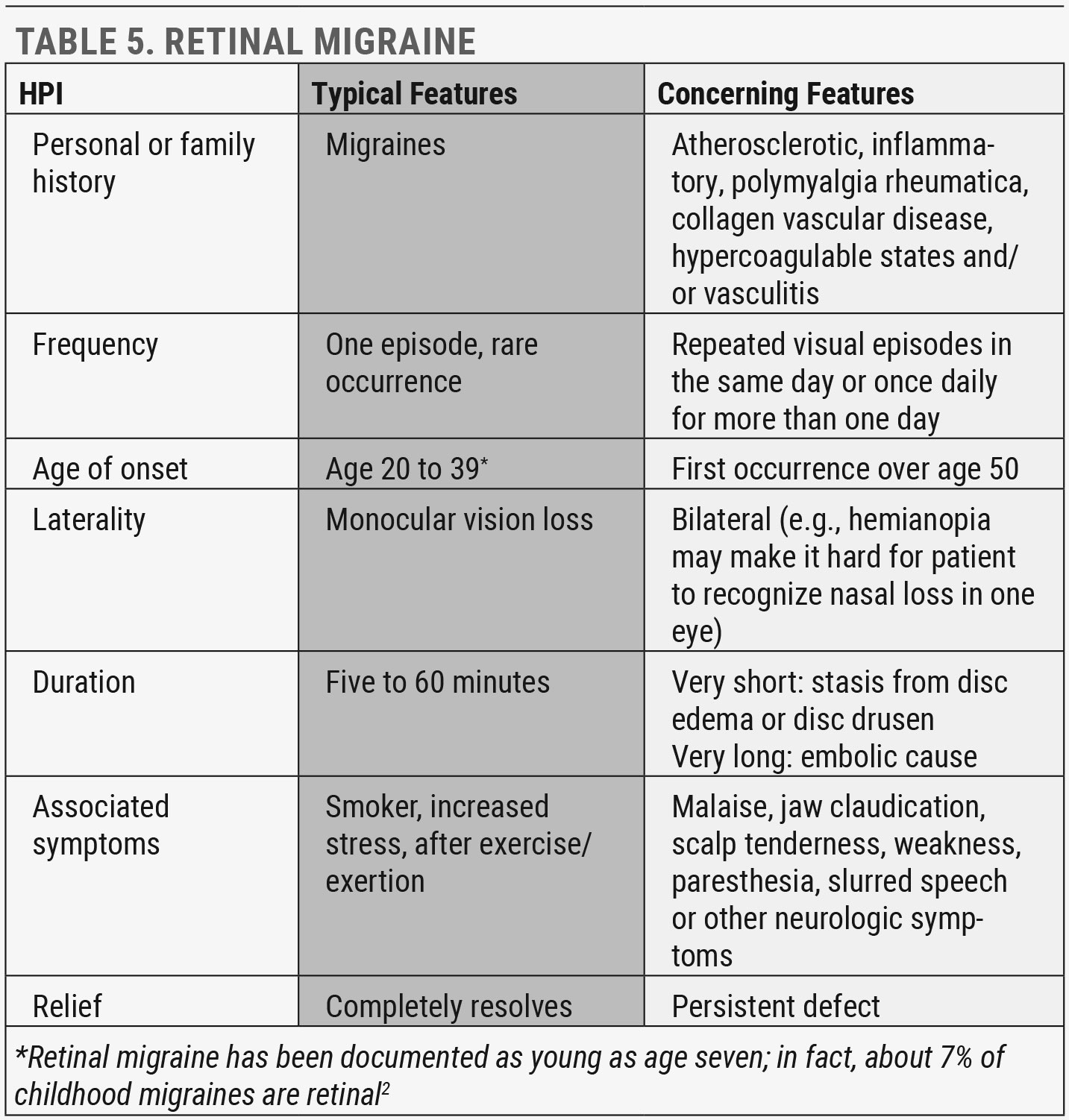 |
| Click table to enlarge. |
which can be a cause of first or recurrent stroke and can also occur as a new condition following a stroke.13
A thorough, unremarkable workup confirms the final diagnosis of retinal, ocular or ophthalmic migraine, but our job is not yet done. Retinal migraine patients are at higher risk for central retinal artery occlusion, central retinal vein occlusion, branch retinal artery occlusion, retinal hemorrhages and/or edema, vitreous hemorrhage, choroidal ischemia, ischemic optic neuropathy and very rarely, permanent vision loss.11 Routine follow-up is necessary, especially when risk factors exist that can increase the possibility of complications.
The terms “retinal,” “ocular” and “ophthalmic” can be used interchangeably; however, they are not to be confused with other migraine aura; specifically, typical aura with or without migraine. Both retinal (ocular or ophthalmic) migraine and typical aura can present with or without headache, and both can have overlapping presentations, but there are key differences in their typical presentation to help guide when a patient should be referred out for further evaluation of retinal migraine. These features include monocular/unilateral, negative aura, complete or incomplete loss of vision, dimming, altitudinal defects and central VF. In comparison, typical visual aura (with or without headache) usually presents with the following: bilateral, positive aura, flashes, scintillations and peripheral VF.
Recognizing the rare migraine complications that require referral is critical. These include status migrainosus, migraine aura-triggered seizure, persistent aura, visual snow, positive lesions on neuroimaging and ischemic lesions on neuroimaging.14
Additionally, retinal migraine should not be confused with previously termed ophthalmoplegic migraine, now more appropriately classified as recurrent painful ophthalmoplegic neuropathy. This disorder involves repeated paresis attacks of one or more ocular cranial motor nerves (III, IV, VI) with ipsilateral headache when brain lesion has been excluded.5
 |
| Click table to enlarge. |
It is estimated that over half of patients with chronic migraine, defined as occurring more than 15 days per month, develop medication overuse headache (MOH), though it’s likely overlooked and misdiagnosed.15 Analgesics, triptans or opiate medications used more than 10 to 15 days per month for more than three months are responsible. The headache usually resolves once overuse is discontinued, but not without side effects. Refer any suspected MOH back to the PCP to help treat the condition.
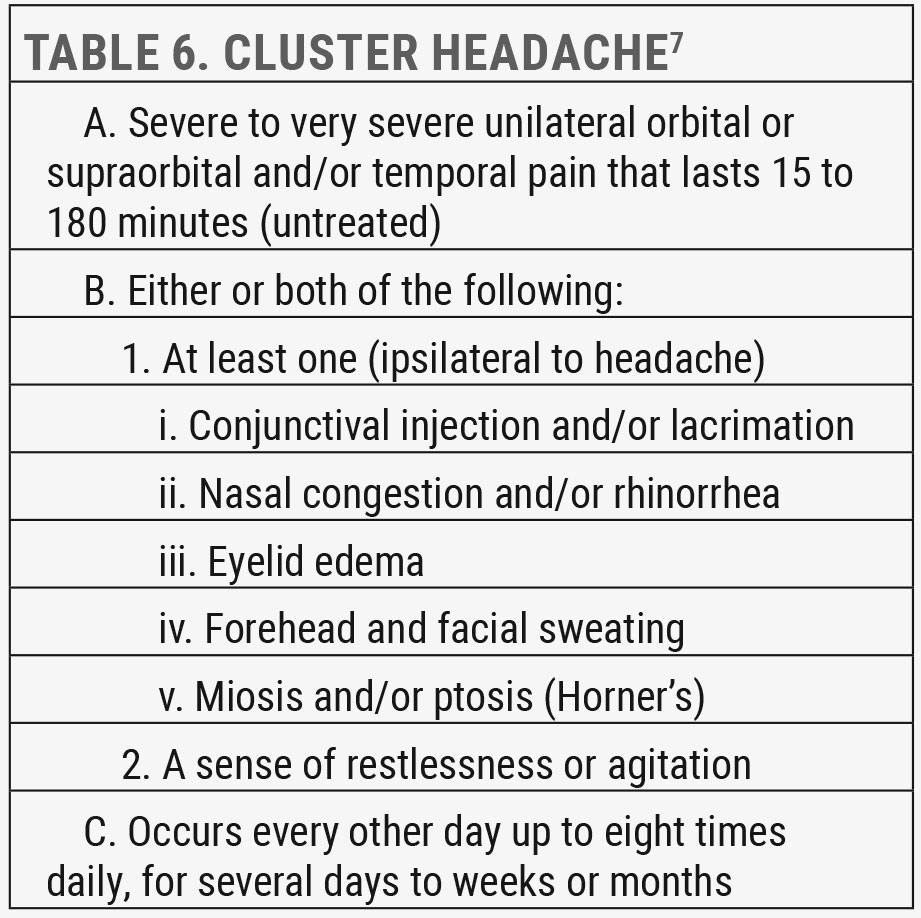
Cluster headaches. This condition is the more common of an otherwise rare headache disorder group TAC, which is broadly characterized by unilateral headache with ipsilateral and prominent cranial, parasympathetic autonomic features. TAC sufferers are more likely to present to us because of involvement of the eye or periorbital region (Table 6).
This disorder appears around age 20 to 40. Unlike the other primary headaches, it is more common in males. Attacks can occur up to eight times daily, repeating on the same side of the head over four to 16 week bouts, once or twice a year. The remission period between these attacks can last months to years but 15% of sufferers have very short or no remission.16
Secondary Headache
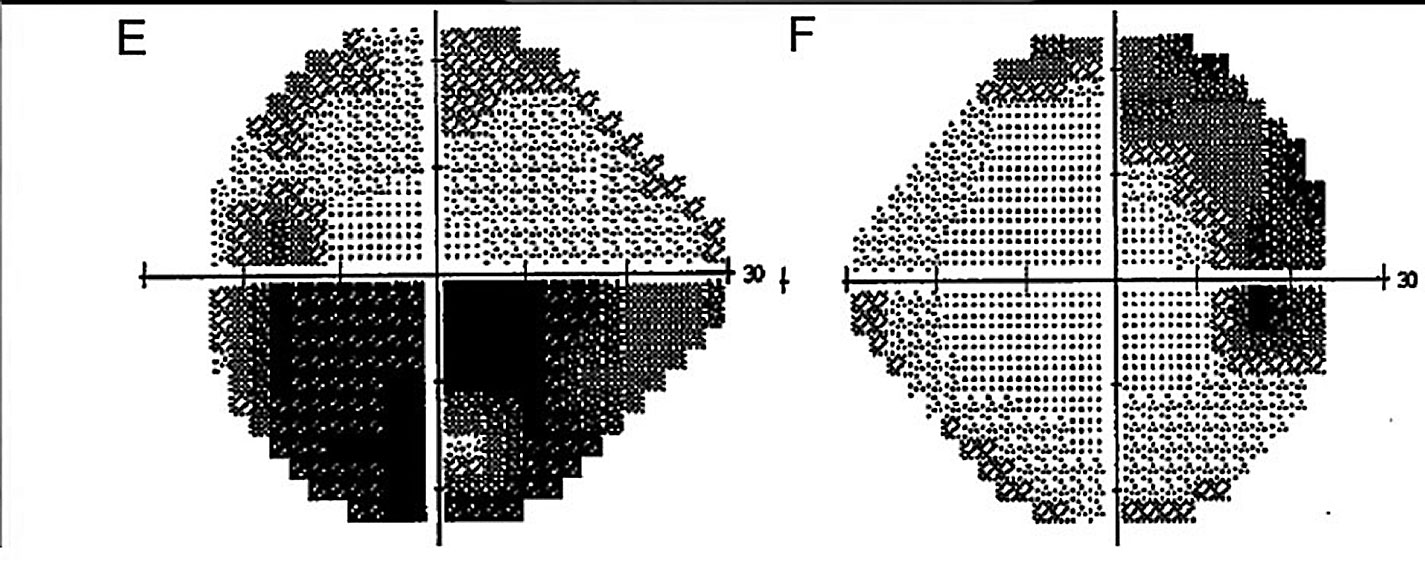 |
| Fig. 5. Humphrey VF 24-2 testing (greyscale) demonstrates a dense, superior arcuate defect in the right eye and a dense, inferior altitudinal defect in the left. Click image to enlarge. |
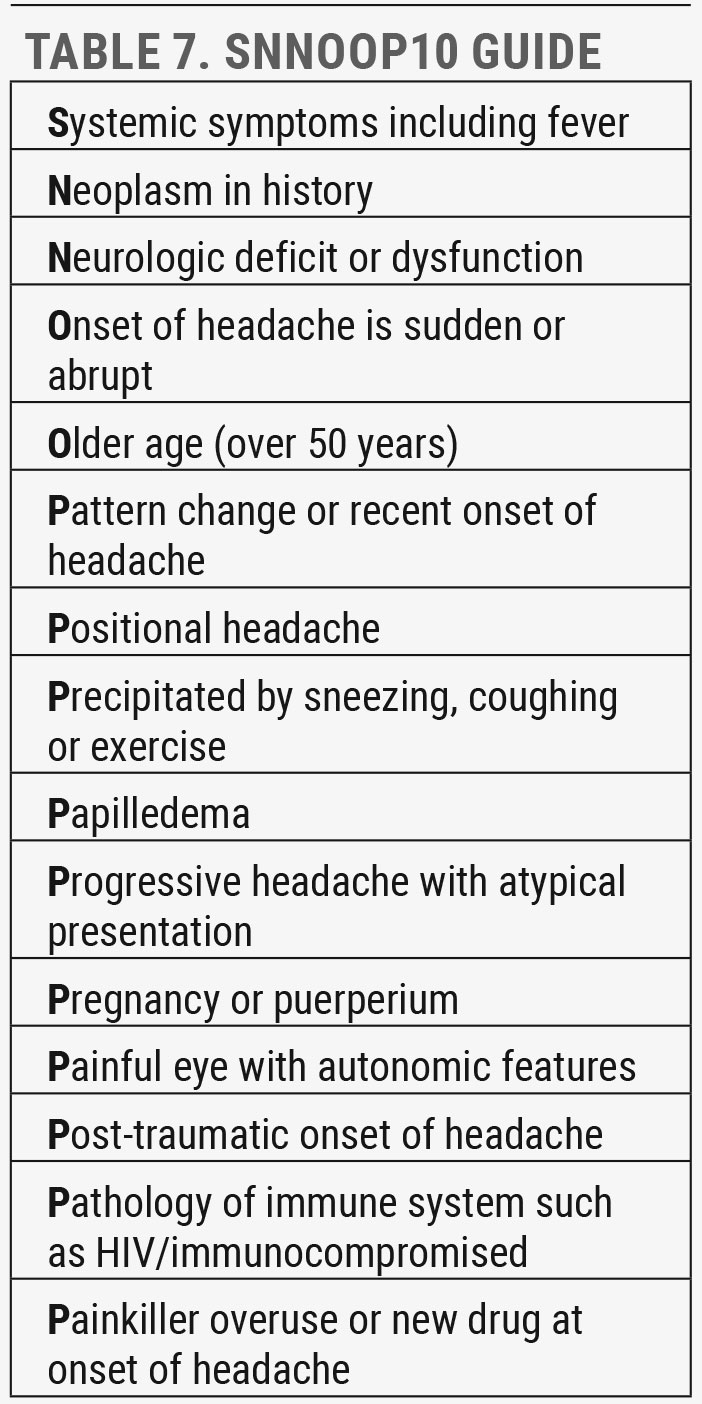
These types of headaches have the potential for significant morbidity and mortality, but only a minority (20% or less) of patients presenting for headache have the secondary type, and an even smaller portion are true emergencies. Use the mnemonic SNNOOP10 as a guide for those red flags that warrant immediate referral to rule out emergent underlying disorders (Table 7).17
Angle closure glaucoma (ACG). This is an important etiology of secondary headache in the ED setting. The association of SSRI and tricyclic antidepressant medications and ACG is low but, given the high prevalence of antidepressant use, one should be suspicious in any patient with new-onset, unilateral headaches and a history of antidepressant medication use. Other medications that can potentially cause ACG include botulinum toxin, anticholinergic agents, antipsychotic agents and sulfa-based agents including topiramate, an anti-epileptic medication that is also often prescribed for migraines.
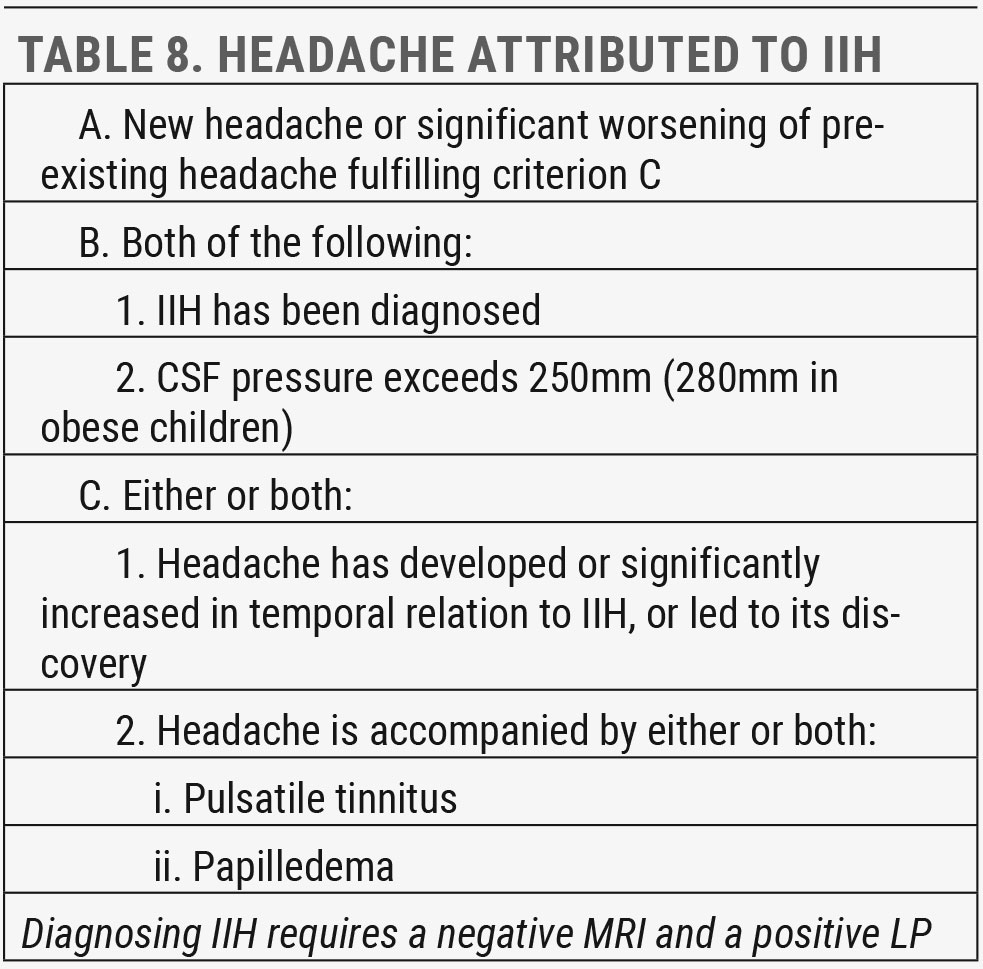
Idiopathic intracranial hypertension (IIH). Drug-induced intracranial hypertension is a known complication in long-term use of anabolic steroids, amiodarone, lithium carbonate, nalidixic acid, thyroid hormone replacement therapy, tetracycline antibiotics, high-dose vitamin A derivatives, estrogen-progestin oral contraceptives and, more recently, antipsychotic medication-induced weight gain, a prominent side effect of first- and second-generation antipsychotics.18
 |
| Click table to enlarge. |
The condition usually has a favorable outcome with spontaneous resolution of papilledema and good visual prognosis once the causative agent is discontinued. Risk factors for more significant vision loss include younger age, higher opening pressure and more severe papilledema.19 When no inducing agent can be identified, the condition is considered IIH (Table 8).
Headache is the most common symptom in IIH, but it presents with a wide variety of characteristics. Some patients describe severe, daily, throbbing headaches that can last for hours and are worsened by postural change, while others may only be mildly symptomatic with vague symptoms.
Transient visual loss, described as obscurations, blurring or darkening, is the second most common symptom, followed by pulsatile tinnitus.20 Other ocular symptoms frequently reported include pain behind the eye or with eye movement and diplopia from CN VI palsy.
IIH is a diagnosis of exclusion that requires negative MRI and positive LP findings. The goal is to treat underlying disease, preserve vision and minimize headache morbidity. Recurrence of IIH is associated with weight gain, so lifestyle interventions for consistent and permanent weight loss are important.
Results from the IIH Treatment Trial demonstrated the importance of maximally tolerated acetazolamide (up to 4g daily) combined with a low-sodium weight loss diet to significantly improve papilledema, lower cerebrospinal fluid (CSF) pressure and improve general and visual quality of life scores. There are still no trials to guide therapy in patients with moderate to severe vision loss who may need surgery.21
If idiopathic intracranial hypertension is suspected or optic disc edema is noted, the following should be documented:
1. Blood pressure (BP)
a. Rule out malignant hypertension, defined as >180/120
2. Ophthalmic examination
a. Visual acuity (VA)
b. Pupils
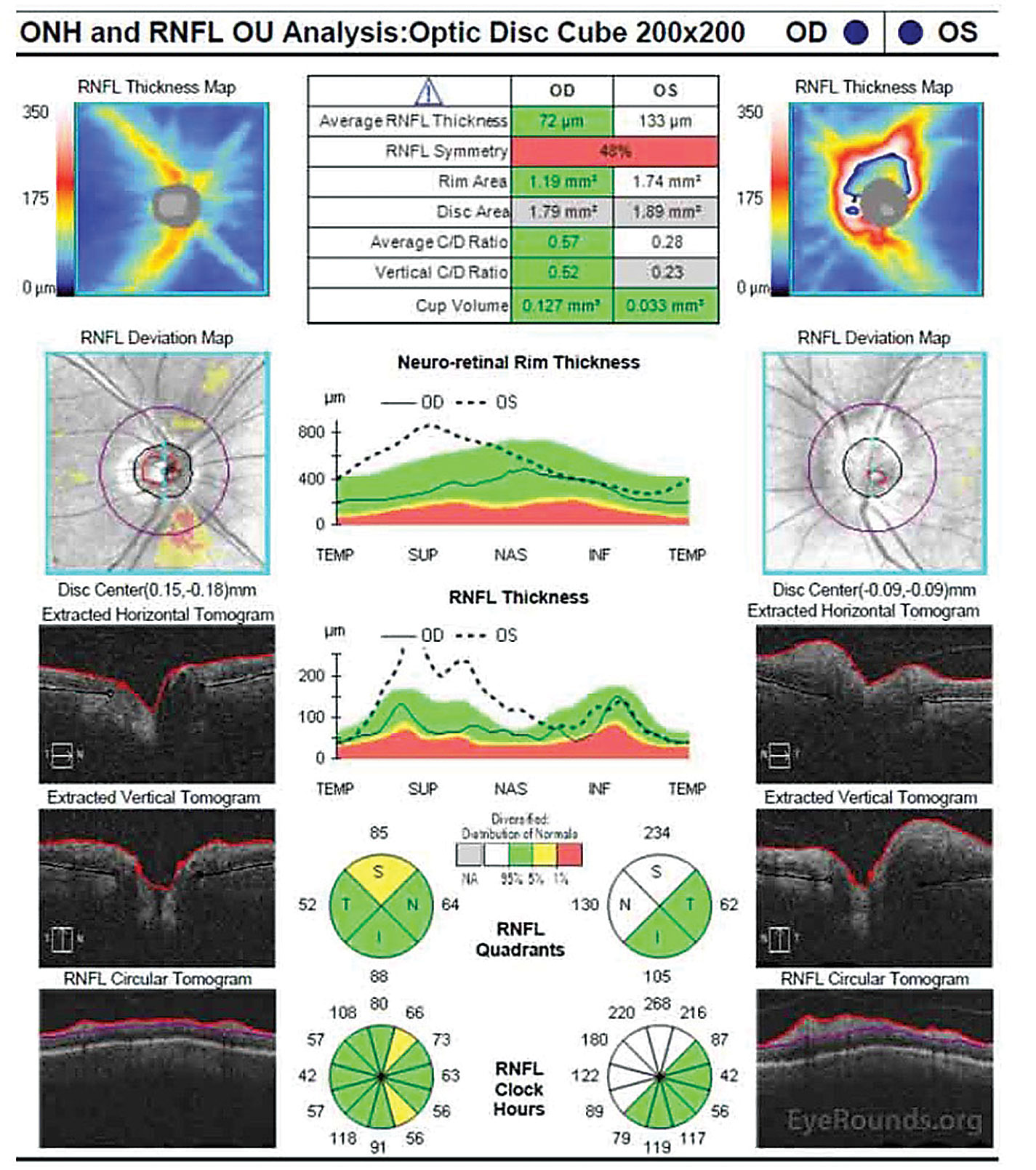 |
| Fig. 6. OCT of the optic nerve shows significantly increased RNFL and neuroretinal rim thickness in the superior and nasal rims OS. Click image to enlarge. |
c. EOM
i. CN VI palsy is more likely to occur
ii. Less frequently CN III, IV palsy
d. VF testing
i. Using dynamic, Goldmann-type or static Humphrey-type
e. Intraocular pressure (IOP)
i. Exclude hypotony, a rare cause of papilledema22
f. Dilated fundus exam
g. Color fundus photos and/or optic nerve OCT to document edema
3. Neurological examination
a. CN VII, IX, XII can also be involved in IIH23
4. Neuroimaging
a. Urgent MRI (with and without contrast) or CT, whichever is available within 24 hours
b. CT or MR venography to exclude cerebral venous sinus thrombosis within 24 hours
5. Once all imaging is confirmed normal, LP >25cm CSF is indicative of IIH20
 |
| Click table to enlarge. |
Meningitis. Headache is the most common presenting symptom of meningitis. The head pain is described as either global or localized to the nuchal area with associated neck stiffness. The classic triad of symptoms associated with meningitis headache—head pain, neck stiffness and fever—are only seen in about half of patients, but at least one occurs in the majority and over 95% present with at least two of the following: head pain, neck stiffness, fever and altered mental status.2
Pending the extent of the infection, there can be neurological symptoms including lethargy, distraction, alterations in mental status, seizure or postictal state. Ophthalmic evaluation may reveal associated optic nerve edema or CN VI palsy from increased intracranial pressure.
Meningitis headache is an emergency. There should be no hesitation in the urgent referral for emergent blood cultures, possible CT before LP and analysis of CSF. Causative agents are bacterial, viral, fungal, parasitic or noninfectious. Bacterial agents are the most concerning since they have the highest mortality rate (approximately 15%).2 Also urgent is differentiating meningitis (inflammation of meninges surrounding the brain and spinal cord) from encephalitis (inflammation of the brain), which presents with more severe neurological symptoms. The prognosis is much worse with encephalitic involvement.
 |
| Click table to enlarge. |
GCA. This condition is a true ocular emergency that requires immediate consultation and treatment. The risk of GCA increases over age 55 but is most common over age 70, with a three-times higher incidence in females. The most commonly reported symptoms are headache, jaw claudication, anorexia/weight loss and scalp tenderness. Other commonly reported symptoms are malaise, myalgia, fever and neck pain.24
The absence of systemic symptoms does not rule out GCA, nor does normal ESR or CRP testing. About 20% of biopsy-positive GCA cases reported vision loss as their sole complaint. Similarly, temporal artery biopsies carry high rates of both false positives and false negatives.25
The main goal of treatment is to prevent further vision loss in the affected eye, decrease the risk to the fellow eye (over half of patients present with contralateral involvement if left untreated) and prevent CVA, heart attack, other cerebral events and dementia.25 Therefore, prompt, high-dose prednisone (1mg/kg per day) is recommended while awaiting test and biopsy results.
Summary
With such a prevalent, universal disorder like headache, it may seem like our role as eye care providers is small. The cases outlined in this article illustrate otherwise. In a review of patients presenting to the ED for headache, 8.5% had relevant ocular fundus abnormalities (retinal hemorrhages, disc edema, disc pallor and grade III/IV hypertensive retinopathy). Of those, 41% had normal neuroimaging studies.26 The authors extrapolate that over 250,000 of the more than three million patients presenting to the ED for headache in the United States have pertinent ocular findings, not including important anterior segment and refractive findings. This highlights the importance of our role in providing comprehensive ophthalmic care for patients suffering from headache.
For case examples, click here.
Dr. Shahid is a clinical associate professor in the Department of Ophthalmology and Visual Sciences at the University of Iowa’s Carver College of Medicine, where she provides comprehensive eye care and vision rehabilitation. She has no financial interests to disclose.
| 1. Rizzoli P, Mullally WJ. Headache. Am J Med. 2018;131(1):17-24. 2. Tabatabai RR, Swadron SP. Headache in the emergency department: avoiding misdiagnosis of dangerous secondary causes. Emerg Med Clin North Am. 2016;34(4):695-716. 3. Saladino RA. Emergency department approach to nontraumatic headache in children. UpToDate. August 13, 2021. www.uptodate.com/contents/emergency-department-approach-to-nontraumatic-headache-in-children. Accessed September 21, 2021. 4. Lee CJ, Felix ER, Levitt RC, et al. Traumatic brain injury, dry eye and comorbid pain diagnoses in US veterans. Br J Ophthalmol. 2018;102(5):667-73. 5. Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia. 2013;33(9):629-808. 6. Beres SJ, Liu GT. New advancements in migraine assessment and treatment. Advances in Ophthalmology and Optometry. 2016;1(1):249-60. 7. Migraine. International Headache Society. 2021. ichd-3.org/1-migraine/. Accessed September 21, 2021. 8. Sinclair AJ, Sturrock A, Davies B, et al. Headache management: pharmacological approaches. Pract Neurol. 2015;15(6):411-23. 9. Øie LR, Kurth T, Gulati S, et al. Migraine and risk of stroke. J Neurol Neurosurg Psychiatry. 2020;91(6):593-604. 10. Rathier L, Roth J. A biobehavioral approach to headache management. R I Med J (2013). 2014;98(2):26-8. 11. Pradhan S, Chung SM. Retinal, ophthalmic, or ocular migraine. Curr Neurol Neurosci Rep. 2004;4(5):391-7. 12. Doyle E, Vote BJ, Casswell AG. Retinal migraine: caught in the act. Br J Ophthalmol. 2004;88(2):301-2. 13. Bonsignore MR, Baiamonte P, Mazzuca E, et al. Obstructive sleep apnea and comorbidities: a dangerous liaison. Multidiscip Respir Med. 2019;14:8. 14. Kruit MC, van Buchem MA, Launer LJ, et al. Migraine is associated with an increased risk of deep white matter lesions, subclinical posterior circulation infarcts and brain iron accumulation. Cephalalgia. 2010;30(2):129-36. 15. Fischer MA, Jan A. Medication-overuse Headache. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021. 16. Wei DYT, Yuan Ong JJ, Goadsby PJ. Cluster headache: epidemiology, pathophysiology, clinical features, and diagnosis. Ann Indian Acad Neurol. 2018;21(5):3-8. 17. Do TP, Remmers A, Schytz HW, et al. Red and orange flags for secondary headaches in clinical practice. Neurology. 2019;92(3):134-44. 18. Namiki H. Antipsychotic pitfalls: idiopathic intracranial hypertension and antipsychotic-induced weight gain. BMJ Case Rep. 2020;13(6): e236161. 19. Saindane AM, Bruce BB, Riggeal BD, et al. Association of MRI findings and visual outcome in idiopathic intracranial hypertension. AJR Am J Roentgenol. 2013;201(2):412-8. 20. Mollan SP, Davies B, Silver NC, et al. Idiopathic intracranial hypertension: consensus guidelines on management. J Neurol Neurosurg Psychiatry. 2018;89(10):1088-100. 21. NORDIC Idiopathic Intracranial Hypertension Study Group Writing Committee. Effect of acetazolamide on visual function in patients with idiopathic intracranial hypertension and mild visual loss. JAMA. 2014;311(16):1641-51. 22. Thomas M, Vajaranant TS, Aref AA. Hypotony maculopathy: clinical presentation and therapeutic methods. Ophthalmol Ther. 2015;4(2):79-88. 23. Thurtell MJ. Idiopathic intracranial hypertension. Continuum (Minneap Minn). 2019;25(5):1289-1309. 24. Mollan SP, Paemeleire K, Versijpt J, et al. European Headache Federation recommendations for neurologists managing giant cell arteritis. J Headache Pain. 2020;21(1):28. 25. Hayreh SS, Zimmerman B. Management of giant cell arteritis. Our 27-year clinical study: new light on old controversies. Ophthalmologica. 2003;217(4):239-59. 26. Thulasi P, Fraser CL, Biousse V, et al. Nonmydriatic ocular fundus photography among headache patients in an emergency department. Neurology. 2013;80(5):432-7. 27. Dahlöf CGH, Johansson M, Casserstedt S, et al. The course of frequent episodic migraine in a large headache clinic population: a 12-year retrospective follow-up study. Headache. 2009;49(8):1144-52. |
