When Drugs Cause Dry Eye
To identify and treat patients more effectively, know these systemic drugs and ocular drops linked to dry eye.
By Juan Ding, OD, PhD
 |
Release Date: October 15, 2019
Expiration Date: October 15, 2022
Estimated Time to Complete Activity: 2 hours
Jointly provided by Postgraduate Institute for Medicine (PIM) and Review Education Group
Educational Objectives: After completing this activity, the participant should be better able to:
- Identify various drug classes, and perhaps some of the most commonly prescribed drugs in particular, that cause or exacerbate dry eye.
- Recognize the possible or theorized mechanisms of action between these drugs and dry eye.
- Effectively alter dry eye treatment to accommodate the patient’s systemic drug regimen.
- Discuss how the patient’s systemic therapy may be modified to better treat dry eye.
Target Audience: This activity is intended for optometrists engaged in the care of patients with dry eye.
Accreditation Statement: In support of improving patient care, this activity has been planned and implemented by the Postgraduate Institute for Medicine and Review Education Group. Postgraduate Institute for Medicine is jointly accredited by the Accreditation Council for Continuing Medical Education, the Accreditation Council for Pharmacy Education, and the American Nurses Credentialing Center, to provide continuing education for the healthcare team. Postgraduate Institute for Medicine is accredited by COPE to provide continuing education to optometrists.
Faculty/Editorial Board: Juan Ding, OD, PhD, UMass Memorial Medical Center, Worcester, MA.
Credit Statement: This course is COPE approved for 2 hours of CE credit. Course ID is 64824-AS. Check with your local state licensing board to see if this counts toward your CE requirement for relicensure.
Disclosure Statements:
Dr. Ding has nothing to disclose.
Managers and Editorial Staff: The PIM planners and managers have nothing to disclose. The Review Education Group planners, managers and editorial staff have nothing to disclose.
We all know that dry eye is one of the most common complaints of patients walking into an eye doctor’s office. Dry eye is associated with older age, the female sex and prolonged use of digital screens. It can also be associated with and exacerbated by certain systemic and ocular medications.
Understanding which medications may affect dry eye helps practitioners identify, diagnose and treat patients’ dry eye more effectively.
 |
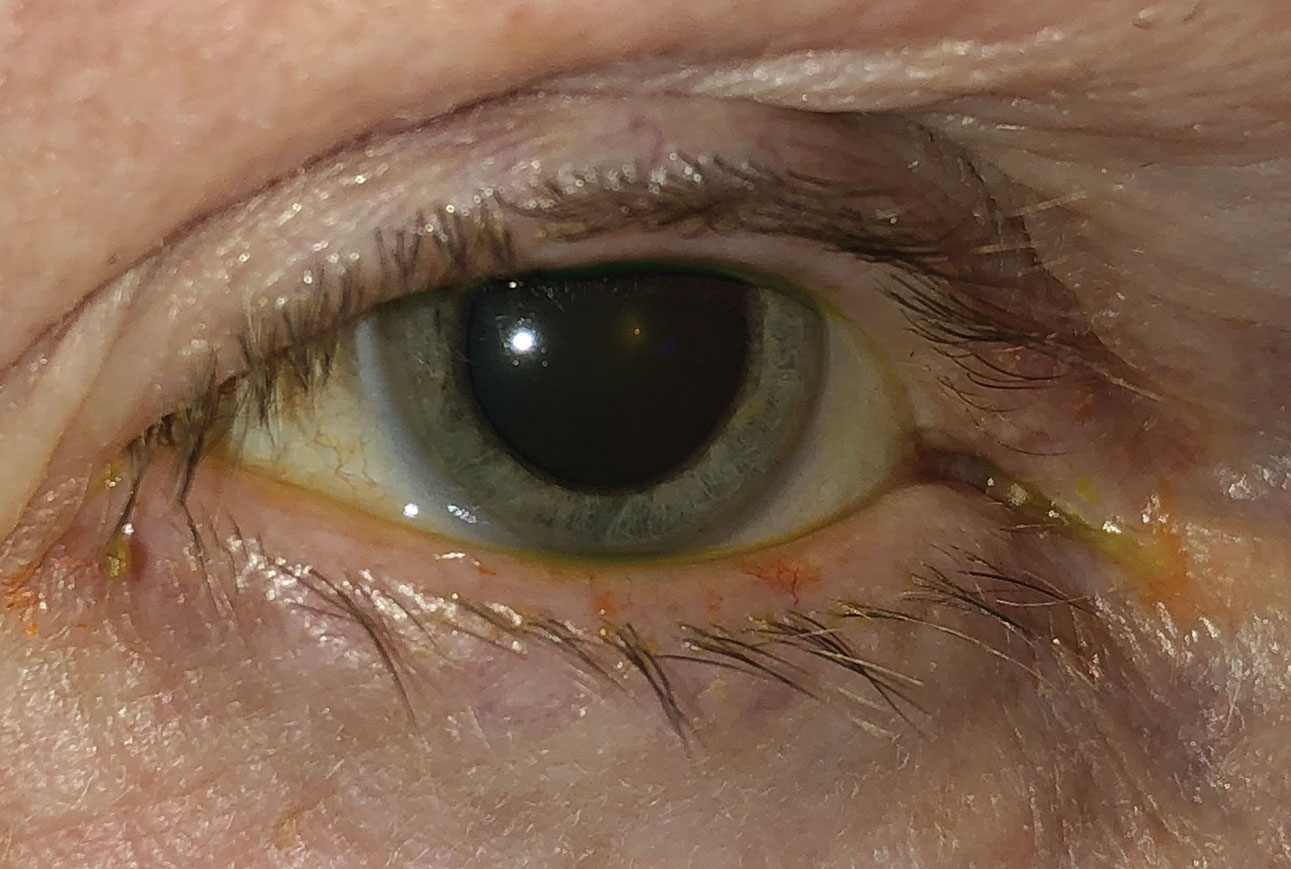
| Corneal superficial punctate keratitis in a young adult taking several antidepressants. Click image to enlarge. |
Systemic Meds That Affect Dry Eye
An estimated 22 of the top 100 best-selling drugs may cause dry eye.1 Overall, 18 classes of drugs can negatively affect dry eye.2 To date, most studies have looked at drug classes, rather than specific drugs, in terms of the effect on dry eye.
Also, most studies only demonstrate association, meaning that dry eye is associated with taking certain drugs, but the research cannot state definitively that dry eye is caused by taking these drugs.
One way of evaluating the risk for developing dry eye when taking a medication is to calculate the odds ratio (OR). An OR of 1 means a patient has equal risk for dry eye when taking this drug compared with patients not taking the medication. The higher the OR, the more likely a drug is associated with dry eye. For example, the odds ratio of antihistamines is 1.67, which means the likelihood of having dry eye when taking antihistamines is 1.67-fold compared with controls.
Table 1 summarizes the odd ratios of certain classes of systemic drugs in the order of highest to lowest OR in relation to dry eye risk. These data are compiled in the Tear Film & Ocular Surface Society (TFOS) Dry Eye Workshop (DEWS) II report on iatrogenic causes of dry eye.2
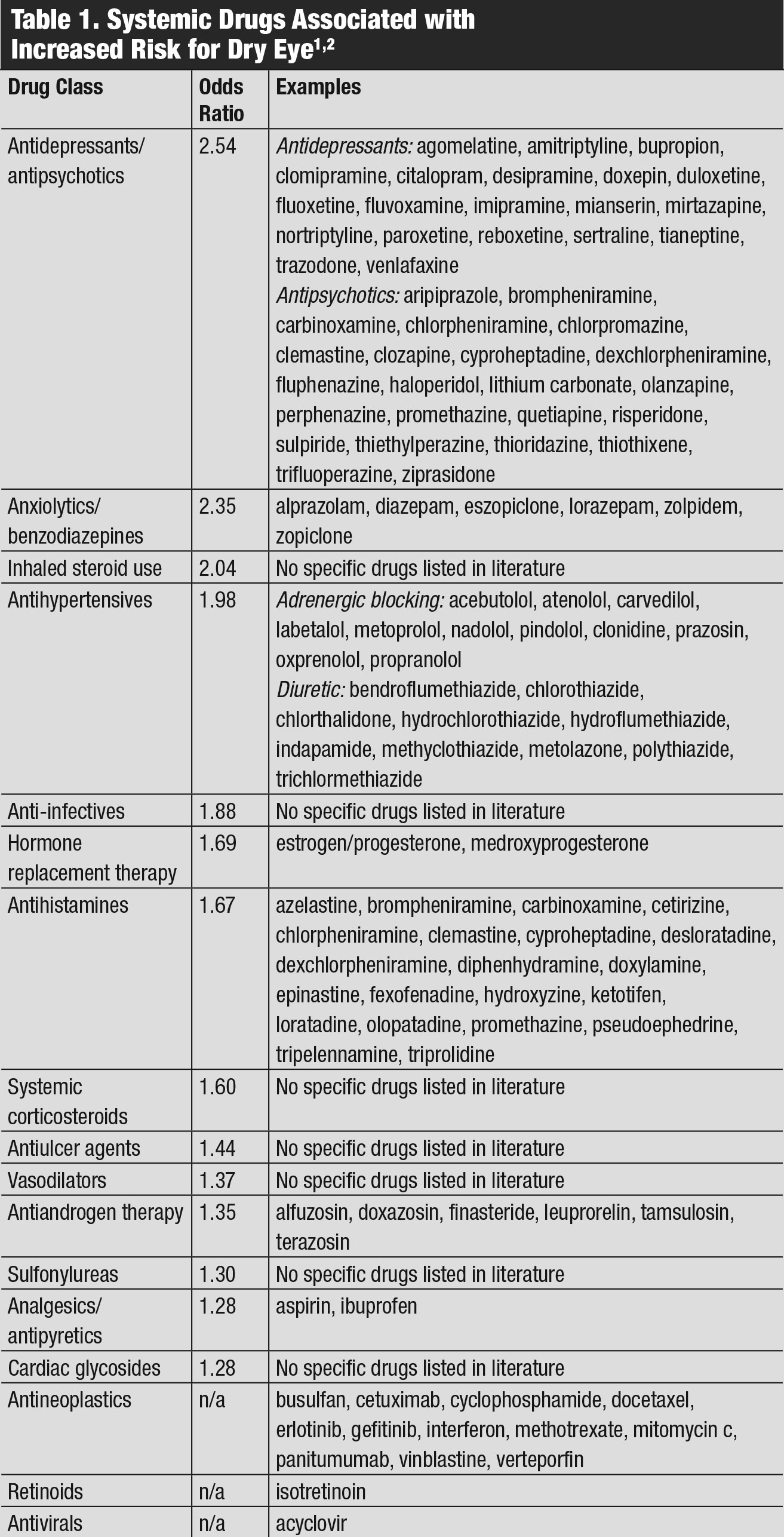 |
| Table 1. Systemic Drugs Associated with Increased Risk for Dry Eye. Click table to enlarge. |
How Systemic Drugs Affect Dry Eye
There are several possible mechanisms by which systemic drugs may cause dry eye: by decreasing tear production; by changing nerve input and reflex secretion; by inducing inflammation on secretory glands; and by direct secretion into the tears.2 Drugs that are secreted into tears include aspirin, chloroquine, clofazimine, docetaxel, ethyl alcohol, hydroxychloroquine, ibuprofen, isotretinoin and amiodarone.1 These may cause mechanical irritation, forming drug crystals or deposits in the tears or cornea, or may result in tear hyperosmolarity.3-5
Anticholinergics and adrenergics. Many systemic drugs have anticholinergic activity, which may explain their sicca effects. The anticholinergic activity can affect lacrimal gland acini, conjunctival mucus-producing cells and meibomian gland epithelial cells via cholinergic receptors.2,6 This leads to reduced tear volume and quality. Drugs with anticholinergic activity include antidepressants, antipsychotics, anti-Parkinson’s drugs, H1-antihistamines, decongestants and benzodiazepines.
On the other hand, adrenergic agents such as beta-blockers and alpha-agonists may cause changes in tear volume and quality, likely mediated by protein kinase C and intracellular calcium concentration.2
Chemotherapeutic drugs. These are known to cause dry eye syndrome. They may do so by inhibiting tear secretion or by affecting the meibomian glands, which are holocrine glands that constantly undergo cell renewal.7 Some chemotherapeutic drugs may also cause blepharitis, such as epidermal growth factor receptor (EGFR) inhibitors and the proteasome inhibitor bortezomib, for example.8 EGFR inhibitors may also impair corneal epithelial healing, leading to corneal epithelial defects.9 Examples of EGFR inhibitors include monoclonal antibodies cetuximab and panitumumab, and the small-molecule EGFR inhibitors erlotinib and gefitinib.
Another dry eye-causing chemotherapy agent is trastuzumab, a monoclonal antibody directed against HER2 and used to treat HER2-overexpresssing breast and gastric cancers.10 Orally available BRAF inhibitors vemurafenib, dabrafenib, and encorafenib—used for treating metastatic melanoma with a BRAFV600 mutation—may also lead to dry eye. Trials of vemurafenib showed that dry eye occurred in 2% and conjunctivitis occurred in 2.8% of those taking it.11
Retinoic acid. Isotretinoin, a form of retinoic acid commonly known by its former brand name Accutane, is used to treat severe acne and certain cancers. Isotretinoin is secreted into the tears by the lacrimal glands and can cause atrophy of the meibomian glands, which can lead to changes in lipid secretion, tear osmolality and tear film stability.12,13
At the molecular and cellular level, research has found that isotretinoin inhibits meibomian gland epithelial cell proliferation, increases cell death, alters the expression of more than 6,000 genes and inactivates important survival signaling pathways.14 Interestingly, isotretinoin has not been proven to directly cause harm to the conjunctiva or cornea, nor does it reduce lacrimal gland tear secretion.2
Sex hormones. Researchers have extensively studied the important role androgens play in ocular surface tissues and dry eye. Androgens are critical in normal functions of the lacrimal glands, meibomian glands, conjunctiva and cornea. Androgen deficiency causes reduced tear volume and tear break-up time, increased meibomian gland disease (MGD) and dry eye signs and symptoms, as reviewed in the TFOS DEWS II Sex, Gender, and Hormones Report.15 In fact, androgen decline with age is a common contributor to the age-related increase in dry eye in both men and women, and research shows androgen decline affects dry eye more than the decline of estrogen and progesterone in menopausal women.15
On the other hand, research shows estrogens have a negative effect on lacrimal glands and possibly meibomian glands as well, though data regarding estrogen is less well defined and appears to depend on sex and dosage.15 For example, high levels of estrogen in hormone replacement therapy (HRT) increases the risk of dry eye.15
Polypharmacy. This refers to concurrent use of five or more medications, whether prescription or over-the-counter (OTC). Most of our knowledge of drug interaction is derived from research that studies two-drug interaction, and little is known about the additive effects when a patient is using three or more drugs.
Researchers suspect that polypharmacy, regardless of which individual drug is used, may increase the risk of dry eye, due to unknown and complicated multi-drug interactions.1 Given that 36.7% of people older than age 60 use more than five drugs, it is no wonder that dry eye in the elderly is further exacerbated by their medication use.17
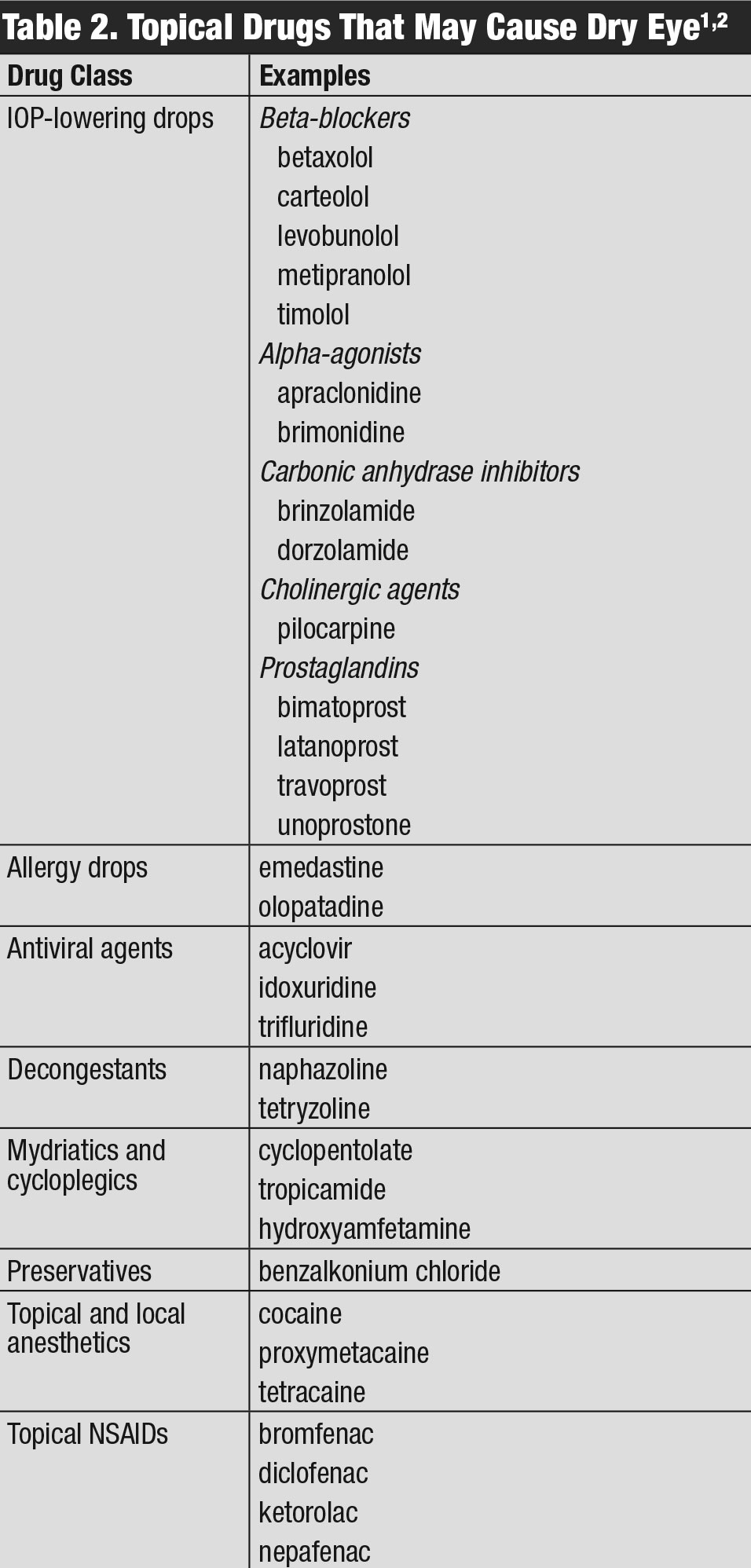 |
| Table 2. Topical Drugs That May Cause Dry Eye. Click table to enlarge. |
Ocular Medications That Affect Dry Eye
In addition to systemic drugs, certain eye drops can also induce or worsen dry eye. These include many popular glaucoma drops, allergy drops, antiviral drops, NSAIDs and common mydriatics that are used diagnostically in our offices (Table 2).
Various eye drops cause allergic, toxic and/or immune/inflammatory effects. This may occur due to the interaction with the tear film and disruption of the lipid layer through detergent effects. These drops can also directly damage goblet cells, the conjunctival and corneal epithelia, corneal nerves and meibomian glands.2
One common ingredient of most preserved eye drops is benzalkonium chloride (BAK), which disrupts the tear film by altering tear film osmolarity.18 BAK also has pro-inflammatory and toxic effects on the ocular surface.19
These cases highlight the link between dry eye and topical medication use:
Case 1. A 25-year-old female complained of blurry vision and difficulty focusing while using a computer for two months. Her medical history was significant for depression and anxiety; she has been on escitalopram and buspirone for six months and omeprazole PRN for acid reflux. Otherwise, she was healthy and not taking any other medications, including OTC. Her entering uncorrected visual acuity was 20/40 in each eye, but with difficulty. Her refractive error was minimal. Her slit lamp exam was remarkable for 3+ corneal superficial punctate keratitis (SPK) in the lower half of both eyes with a reduced tear meniscus. Her eye examination was otherwise unremarkable.
She was started on OTC artificial tears in both eyes four times a day and warm compress of eyelids twice a day. She was scheduled to return in two weeks for follow up.
At the next visit, her visual acuity had improved to 20/30 and the SPK significantly improved to grade 1. Accommodative dysfunction was suspected due to her ability to see 20/20 with only +0.25-0.25x180.
Sure enough, her accommodative amplitude was 4D in each eye and NRA/PRA at +2.00/-1.25. Given this finding, PALs were prescribed with distance MRx and +1.50 add. Since her dry eye was well controlled, she was instructed to continue the artificial tears and warm compress, and was scheduled for follow up in three months. If her dry eye gets worse, meibography may be employed to examine the health status of the meibomian gland. Because 70% of dry eye has an MGD component, it is often necessary to treat MGD to treat dry eye successfully long-term.
Escitalopram and buspirone are commonly prescribed antidepressants. As discussed earlier, certain antidepressants have the potential to cause dry eye. In addition, they can affect the accommodative system of the eye.20 We should be on the lookout when a young and otherwise healthy patient presents with dry eye and/or accommodative dysfunction for a possible association with their antidepressant use.
Case 2. A 31-year-old female patient with cutaneous melanoma was taking dabrafenib and trametinib for four months before developing redness, photophobia and mild eye pain. Her ocular exam revealed bilateral iritis as well as dry eye. Her iritis resolved with 1% prednisolone acetate, but her dry eye persisted. Fortunately, the dry eye responded well to preservative-free artificial tears.
Dabrafenib is known to cause uveitis, but an often-overlooked side effect is dry eye. In drug-induced uveitis such as this, we should also check for dry eye, which sometimes causes persistent symptoms even after uveitis is resolved.
Case 3. A 25-year-old male graduate student took isotretinoin for six months to treat acne. Afterwards, he developed persistent dry eye. He has tried numerous OTC artificial tears, warm compresses, punctal plugs, autologous serum drops, meibomian gland probing and LipiFlow (Johnson & Johnson Vision), but is still battling with pain and burning every day. This case exemplifies how extremely challenging it can be to treat MGD induced by isotretinoin.
Case 4. A 70-year-old female with ocular rosacea and nasal allergies complained of a gritty feeling and tearing of both eyes for one year. She is a classic example of a patient at increased risk for developing dry eye from ocular rosacea alone. Added to this, she’s taking antihistamines orally for her longstanding allergies, which has further exacerbated the dry eye.
In situations such as this, we should let patients know of the multiple risk factors for dry eye, implement more aggressive dry eye management and stress the importance of consist day-to-day eyelid hygiene and use of lubrication.
 |
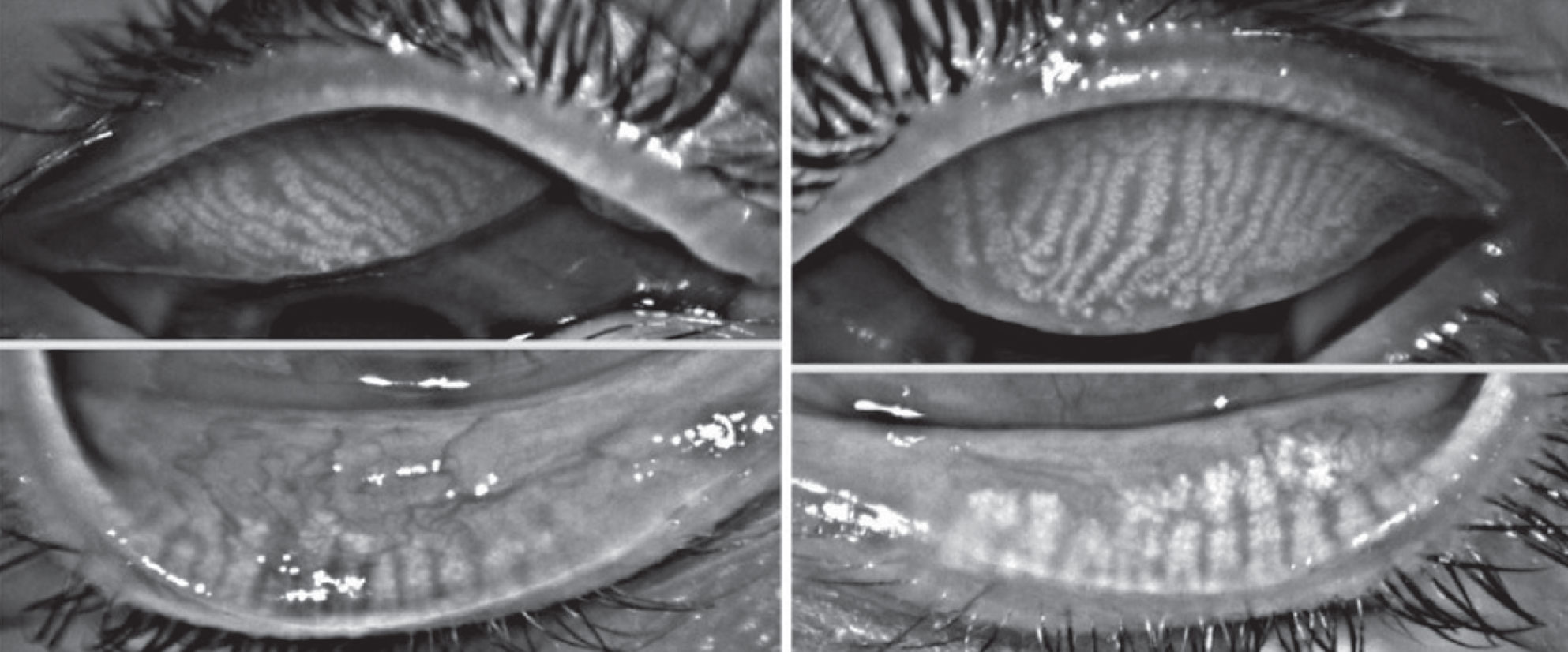
| This patient has both ocular rosacea and dry eye. Click image to enlarge. |
Treating Drug-Related Dry Eye
We can treat iatrogenic dry eye with various therapies. First line is artificial tears and eyelid hygiene. If these are not adequate to control dryness, a topical steroid may be used in the short term, as well as Restasis (cyclosporine 0.05%, Allergan) and Xiidra (lifitegrast 5%, Novartis) long-term.
Punctal plugs are good options for aqueous-deficient dry eye. But for the majority of patients who have evaporative dry eye, MGD may be treated with LipiFlow, TearCare (Sight Sciences), iLux (Alcon) or another targeted heat delivery system to the eyelids. For dry eye patients with rosacea, intense pulsed light can be especially helpful. Finally, for severe dry eye, amniotic membrane, autologous serum drops and therapeutic scleral lenses may provide relief.
Patient education is key. Rather than brushing off patients with comments such as, “you just have some dry eye,” it is usually better to offer an explanation as to why they are suffering from the condition. For example, you should explain the impact of HRT on dry eye to a postmenopausal woman on HRT who has an exacerbation of dry eye for a few months. The treatment may not necessarily discontinue, but the patient should understand that the gritty feeling in her eyes may be expected, and that she should follow the recommended dry eye treatment.
Consider the following alternatives for patients with dry eye-related to systemic medications:
• Change to another drug (class). This is a nice concept but sometimes difficult in practice. Again, most research looks at drug class rather than individual drugs, making it hard to know which drug may be a better choice; perhaps the entire class will have similar effects on dry eye. Changing medications is certainly worth trying and perhaps for a given patient, an effective drug can be found that lessens dry eye problems. It is important to communicate with the patient’s primary care provider or treating physicians for alternative medications that may have fewer dry eye effects.
• Reduce dosage. A reduced medication dosage may be achievable if the medication is still effective in treating the patient’s main health condition. As optometrists, we should communicate with the treating physician to see if a reduced dosage is possible.
• Change dosing time schedule. If a patient’s medication does not require a specific time to take, we may advise the patient to take it at a different time to avoid peak concentration or side effects that may interfere with their daily activities. For example, certain medications may be taken before bed rather than in the morning so that the dry eye effect occurs while the eyes are shut, reducing the effect on daily activities such as driving or working.
• Discontinue a medication. The determination to switch or terminate a medication suspected to cause dry eye has to be on a case by case basis. For example, chemotherapeutic drugs are rarely worth stopping to alleviate the comparatively minor side effect of dry eye.
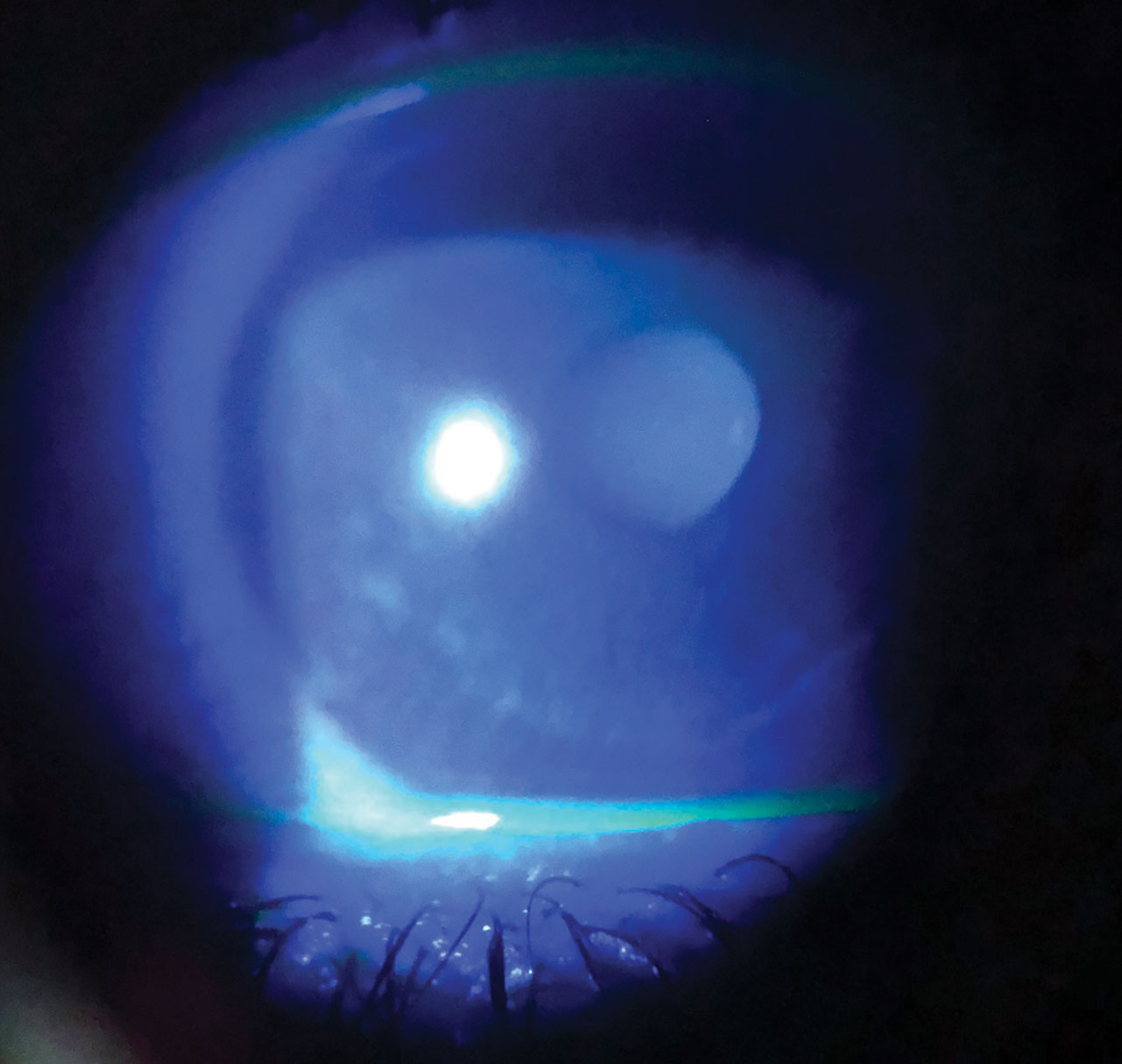 |
| Dry eye in a patient with melanoma taking chemotherapeutic medications. Click image to enlarge. |
For acne, isotretinoin is usually reserved for severe forms and typically for younger patients. The duration of isotretinoin therapy is typically four to six months. The long-term compromise in patient quality of life would be devastating if they develop irreversible MGD from this treatment. Although some patients’ dry eye will resolve a few months after discontinuation of isotretinoin, for some the dry eye persists for many years or may be permanent.12 One retrospective study evaluating 1,741 subjects on Accutane discovered that 1% of these patients developed irreversible dry eye.21
Some dermatologists send patients for an eye evaluation prior to initiating isotretinoin therapy. This examination should include a careful examination of the patient’s ocular surface, including the meibomian glands, and a check for other dry eye contributing medications. If no pre-existing MGD or dry eye exist, and the patient is not on other medications that may be related to dry eye (e.g., antidepressants or antihistamines), you may decide to clear the patient for the therapy, with close monitoring of ocular surface signs and meibomian gland evaluation.
Should early signs of dry eye emerge, the patient should start immediate dry eye therapy such as artificial tears, eyelid hygiene and MGD treatment. Communicate with the treating dermatologist to seek alternative therapy.
For patients with dry eye related to topical ocular drops, consider the following options:
• Switch to a drop with a different preservative. One major issue for chronic eye drop users is the preservatives in the drops. Glaucoma patients may need to be on IOP-lowering drops for decades, and many patients develop redness/irritation after instilling drops. Several IOP-lowering drops employ preservatives other than BAK, which may be better tolerated than BAK-containing drops and may serve as alternative medications for glaucoma. Travatan Z (travoprost, Novartis) is preserved with SofZia, which contains borate, zinc and sorbitol. Alphagan P (brimonidine, Allergan) is preserved with Purite, a stabilized oxychloro complex that has broad antimicrobial activity through oxidative damage. While these have lower toxic activities than BAK, the TFOS DEWS II Iatrogenic Report cautions that they have not been fully investigated in terms of dry eye.2
• Go preservative free. Preservative-free glaucoma drops are also available, which can be much better for dry eye. Examples include Zioptan (tafluprost, Akorn), Cosopt PF (dorzolamide-timolol, Akorn) and Timoptic in Ocudose (timolol maleate, Valeant Pharmaceuticals).
• Consider surgery. The problem with preservative-free glaucoma drops is that they can be much more costly than preserved ones. Patients may save opened containers, which may lead to contamination. Other alternatives include laser procedures, such as selective laser trabeculoplasty or minimally invasive glaucoma surgeries to reduce drop dependence.
• Switch allergy drops and/or add artificial tears. Another ocular med that may be used long-term is an allergy drop. For patients with allergic conjunctivitis, these may be used for months or even year-round. If dry eye gets worse while on olopatadine or emedastine, for example, consider alternative drops such as ketotifen, azelastine, epinastine, alcaftadine or bepotastine.
If a patient has concurrent allergy and dry eye, always tell them to use artificial tears as well, and educate patients that their allergy drops will not help with dry eye, and their dry eye needs to be managed in addition to their allergies.
• Advise against red eye-reducing drops. For patients with allergies or chronic red eyes, another potentially abused eye drop is OTC redness relievers containing decongestants such as naphazoline and tetryzoline. As optometrists, we should inform patients that these drops will not only cause rebound redness if used long term, but also may cause dry eye, making their symptoms worse.
A good redness-relieving drop that does not cause rebound redness is Lumify (brimonidine, Bausch + Lomb), now available OTC, which patients can use in conjunction with other dry eye treatments.
 |
| This is what Accutane-induced dry eye looks like on meibography.12 Photo: Nancy Mcnamara, OD, PhD. Click image to enlarge. |
We live in a world of pharmaceuticals, where almost every medical condition has a potential solution involving pills, drops, injectables, inhalers, transdermal patches or other delivery methods. Unfortunately, dry eye—the number one reason patients visit eye care practitioners—is affected by a multitude of drugs, both prescription and OTC.
As optometrists, we are in a unique position to help patients find possible causes of their dry eye. One of the ways we do that is by knowing the ever-increasing list of medications that can induce or aggravate dry eye. This is essential to providing patients with proper education and successful dry eye treatment.
Dr. Ding is an assistant professor in the Department of Ophthalmology & Visual Sciences at the University of Massachusetts Medical School and started the optometric service at the Eye Center at UMass Memorial Medical Center. She has conducted and published research on dry eye disease and MGD, and was a coauthor of the TFOS Dry Eye Workshop II 2017.
1. Fraunfelder FT, Sciubba JJ, Mathers WD. The role of medications in causing dry eye. J Ophthalmol. 2012;2012:285851. 2. Gomes JAP, Azar DT, Baudouin C, et al. TFOS DEWS II iatrogenic report. Ocul Surf. 2017;15(3):511-38. 3. Valentic JP, Leopold IH, Dea FJ. Excretion of salicylic acid into tears following oral administration of aspirin. Ophthalmology. 1980;87(8):815-20. 4. Dickinson EJ, Wolman RL. Drug points: Sicca syndrome associated with amiodarone therapy. Br Med J (Clin Res Ed). 1986; 293(6545):510. 5. Kim JH, Kim JH, Nam WH, et al. Oral alcohol administration disturbs tear film and ocular surface. Ophthalmology. 2012 May;119(5):965-71. 6. Kam WR, Sullivan DA. Neurotransmitter influence on human meibomian gland epithelial cells. Invest Ophthalmol Vis Sci. 2011;52(12):8543-8. 7. Bron AJ, de Paiva CS, Chauhan SK, et al. TFOS DEWS II pathophysiology report. Ocul Surf. 2017;15(3):438-510. 8. Liu CY, Francis JH, Pulido JS, et al. Ocular side effects of systemically administered chemotherapy. UpToDate.com. www.uptodate.com/contents/ocular-side-effects-of-systemically-administered-chemotherapy. April 23, 2019. Accessed September 19, 2019. 9. Borkar DS, Lacouture ME, Basti S. Spectrum of ocular toxicities from epidermal growth factor receptor inhibitors and their intermediate-term follow-up: a five-year review. Support Care Cancer. 2013;21(4):1167-74. 10. Camidge DR, Bang YJ, Kwak EL, et al. Activity and safety of crizotinib in patients with ALK-positive non-small-cell lung cancer: updated results from a phase 1 study. Lancet Oncol. 2012;13(10):1011-9. 11. Choe CH, McArthur GA, Caro I, et al. Ocular toxicity in BRAF mutant cutaneous melanoma patients treated with vemurafenib. Am J Ophthalmol. 2014;158(4):831-37. 12. Moy A, McNamara NA, Lin MC. Effects of isotretinoin on meibomian glands. Optom Vis Sci. 2015;92(9):925-30. 13. Knop E, Knop N, Millar T, et al. The international workshop on meibomian gland dysfunction: report of the subcommittee on anatomy, physiology, and pathophysiology of the meibomian gland. Invest Ophthalmol Vis Sci. 2011;52(4):1938-78. 14. Ding J, Kam WR, Dieckow J, Sullivan DA. The influence of 13-cis retinoic acid on human meibomian gland epithelial cells. Invest Ophthalmol Vis Sci. 2013;54(6):4341-50. 15. Sullivan DA, Rocha EM, Aragona P, et al. TFOS DEWS II Sex, Gender, and Hormones Report. Ocul Surf. 2017;15(3):284-333. 16. Schaumberg DA, Buring JE, Sullivan DA, Dana MR. Hormone replacement therapy and dry eye syndrome. JAMA. 2001;286(17):2114-9. 17. Gu Q, Dillon CF, Burt VL. Prescription drug use continues to increase: US prescription drug data for 2007-2008. NCHS Data Brief. 2010;(42):1-8. 18. Labbé A, Terry O, Brasnu E, et al. Tear film osmolarity in patients treated for glaucoma or ocular hypertension. Cornea. 2012;31(9):994-9. 19. Baudouin C, Labbé A, Liang H, et al. Preservatives in eyedrops: The good, the bad and the ugly. Prog Retin Eye Res. 2010;29(4):312-34. 20. Mazow ML, France TD, Finkleman S, et al. Acute accommodative and convergence insufficiency. Trans Am Ophthalmol Soc. 1989;87:158-68. 21. Fraunfelder FT, Fraunfelder FW, Edwards R. Ocular side effects possibly associated with isotretinoin usage. Am J Ophthalmol. 2001;132(3):299-305. |
