 |
Piecing Together the HSVK Puzzle
Given the seriousness of this condition, proper differential diagnosis and medical management is key.
By Alexander Martinez, OD, and Shannon K. Leon, OD
Release Date: April 15, 2022
Expiration Date: April 15, 2025
Estimated Time to Complete Activity: 2 hours
Jointly provided by Postgraduate Institute for Medicine (PIM) and Review Education Group
Educational Objectives: After completing this activity, the participant should be better able to:
- Understand the presentations of herpes simplex virus keratitis.
- Distinguish between HSVK and differential diagnoses.
- Diagnose patients with herpes simplex virus keratitis.
- Medically manage herpes simplex virus keratitis cases.
Target Audience: This activity is intended for optometrists engaged in managing herpes simplex virus keratitis patients.
Accreditation Statement: In support of improving patient care, this activity has been planned and implemented by PIM and the Review Education Group. PIM is jointly accredited by the Accreditation Council for Continuing Medical Education, the Accreditation Council for Pharmacy Education and the American Nurses Credentialing Center to provide CE for the healthcare team. PIM is accredited by COPE to provide CE to optometrists.
Reviewed by: Salus University, Elkins Park, PA
Faculty/Editorial Board: Alexander Martinez, OD, and Shannon K. Leon, OD
Credit Statement: This course is COPE approved for 2 hours of CE credit. Activity #123706 and course ID 77908-TD. Check with your local state licensing board to see if this counts toward your CE requirement for relicensure.
Disclosure Statements: PIM requires faculty, planners and others in control of educational content to disclose all their financial relationships with ineligible companies. All identified conflicts of interest are thoroughly vetted and mitigated according to PIM policy. PIM is committed to providing its learners with high-quality, accredited CE activities and related materials that promote improvements or quality in healthcare and not a specific proprietary business interest of an ineligible company.
Those involved reported the following relevant financial relationships with ineligible entities related to the educational content of this CE activity: Authors: Drs. Martinez and Leon have no financial interests to disclose. Managers and Editorial Staff: The PIM planners and managers have nothing to disclose. The Review Education Group planners, managers and editorial staff have nothing to disclose.
 |
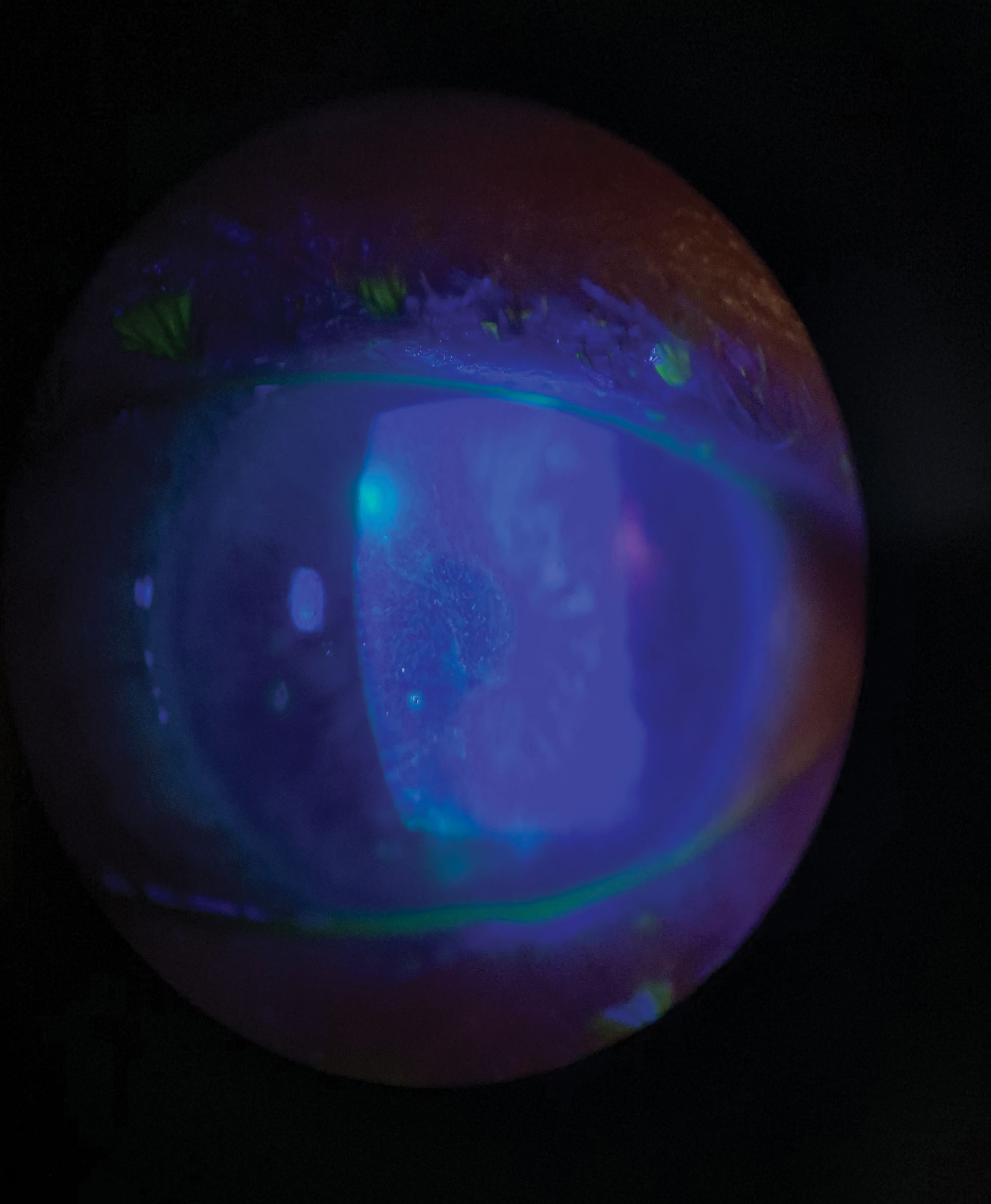
| Epithelial disease presents with dendritic lesions that are characteristic of the condition. Click image to enlarge. |
Throughout our careers as eyecare professionals, we encounter many concerning conditions with the potential for devastating visual outcomes. One in particular is the often-frustrating herpes simplex virus keratitis (HSVK). Due to its varied presentation and recurrence rate, delays in proper diagnosis and treatment often lead to corneal scarring and poor visual outcomes. Thus, it has become increasingly important to recognize the signs and symptoms of this condition and promptly initiate appropriate management. By increasing our understanding of HSVK, we can improve our patients’ overall comfort and their visual prognosis.
Understanding the Virus
To truly recognize why HSVK can be so visually devastating, we must first understand the pathophysiology that makes this pathogen so prevalent.
The herpes simplex virus (HSV) is a linear, double-stranded DNA virus that belongs to the Herpesviridae family.1 There are over 100 known herpes viruses within this family, including HSV-1, HSV-2, varicella-zoster virus, cytomegalovirus and the Epstein-Barr virus.2
HSV is unique in its ability to reproduce quickly in a variety of tissues and establish latency, which can be reactivated at a later time.3 This has resulted in HSVK becoming the leading cause of infectious corneal blindness among developed nations.3 In fact, over 10 million people worldwide may have herpetic eye disease, with the seroprevalence being over 50% in the United States alone.3
HSV-1 is the most common serotype associated with ocular infections. Ocular involvement rarely stems from HSV-2, a disease typically sexually transmitted through the transferral of infected secretions.3 There are two main stages of infection in the pathophysiology of HSV-1: primary infection and reactivation (or recurrence).3 Primary infection occurs through direct contact with mucous membranes of the face, lips or eyes due to trigeminal nerve innervation of all three structures. These primary infections commonly cause contagious cold sores or fever blisters in and around the mouth. They rarely involve the cornea.3,4 Signs and symptoms of corneal manifestations associated with this phase of the infection are often subclinical and mild.3
Once a primary infection occurs in the mucous membrane of the eye, the virus then travels down to the trigeminal ganglion, where it becomes latent.3 Any event that stresses the immune system, whether it be physiological (e.g., fever) or otherwise (e.g., environmental stressors), can then result in reactivation of the latent virus.3 After the virus is reactivated it travels along the ophthalmic branch of the trigeminal ganglion to the cornea, resulting in either superficial epithelial replication, which presents as dendritic keratitis, or in an immune-mediated response (stromal or endothelial keratitis).3
 |
| Use of vital dye staining is extremely helpful in distinguishing dendrites and making an accurate diagnosis. Click image to enlarge. |
Making the Correct Diagnosis
HSVK can have various clinical manifestations, making it challenging for the clinician to determine a proper diagnosis. It is essential to first obtain a thorough case history to gather any relevant information that can assist in the diagnosis. Important questions to ask include recent use of topical or oral corticosteroids, ocular trauma, ocular surgeries, psychological stress, history of HSVK, recent illnesses, fever, extraordinary ultraviolet light exposure, immunosuppression, history of sexually transmitted diseases and hormonal changes.5-7 Physical stimuli, emotional triggers and corticosteroid use can weaken the immune system, allowing the virus to reactivate and causing ocular HSV.
Next, a gross examination of the facial adnexa can reveal vesicles on the forehead, eyelids or nose that may respect the vertical midline, which would narrow down the diagnosis to herpes zoster ophthalmicus, not HSVK. The latter typically presents with an acute onset of symptoms of unilateral ocular pain, redness, photophobia, tearing, itching, foreign body sensation, irritation and blurred vision.1
HSVK can usually be diagnosed with a slit lamp biomicroscopy exam alone and without any laboratory testing. Corneal sensitivity evaluation is also important and is easily performed using a cotton wisp by first testing the unaffected cornea to determine any differences in corneal sensation compared with the non-affected eye. Decreased corneal sensation is a hallmark for herpetic keratitis, unlike other microbial infections where there is an increase in sensation.8
Corneal sensory loss is a common sequela from both herpes simplex keratitis and herpes zoster ophthalmicus, with more severity in the latter.9 The degree of corneal sensory loss is directly proportional to the number of recurrences.9 During the slit lamp examination, dyes such as fluorescein, rose bengal and lissamine green are essential in assisting the clinical diagnosis of HSVK. Corneal dendrites are easily seen with fluorescein dye, since the body of the dendrite will illuminate as there is epithelial breakdown and decaying cells present. On the other hand, rose bengal and lissamine green will stain the dendrite’s viral infected cells at the margins of the swollen terminal bulbs.6,7,10
These dyes also assist the clinician in correctly distinguishing a corneal dendrite from a pseudodendrite caused by herpes zoster ophthalmicus. Pseudodendrites have raised centers filled with swollen cells without terminal bulbs, ulceration or branching.11,12 These epithelial cells are not adherent, typically seen in the periphery and appear to be stuck.11,12 They also stain poorly with vital dyes, producing a negative staining with fluorescein and rose bengal.6,12
A slit lamp examination is typically sufficient in diagnosing HSVK; however, laboratory and diagnostic tests are available for atypical cases where a diagnosis of HSVK cannot easily be made. The main diagnostic tests for HSVK include culturing, direct fluorescent antibody (DFA) and polymerase chain reaction (PCR). Other, less commonly used diagnostic tests include cytology, enzyme-linked immunosorbent assay and serology.13
Culturing HSV-1 is considered the gold standard. Culturing a virus is a misnomer as a virus cannot grow on a culture plate of agar but can infect other cells on the plate, thus proliferating the virus. Only cases of HSV epithelial keratitis can be cultured, since a virus cannot be cultured from the stroma or endothelium.6,13 Culturing tends to have high specificity and low sensitivity and typically takes up to 10 days to obtain the results.13
DFA and PCR have proven to be reliable alternatives in determining the presence of HSV-1. DFA detects any HSV-1 antigens and provides rapid results with lower specificity than PCR, which detects viral DNA and is shown to be as sensitive and specific as a cell culture.13 A limitation of PCR is its inability to differentiate between pathological levels of HSV and normal shedding of HSV in the tear film.13 Serology is not commonly used, since a majority of people have already had prior exposure to HSV; thus, it has low specificity.8,13 Serology is more useful in younger patients where primary infections are more common.13
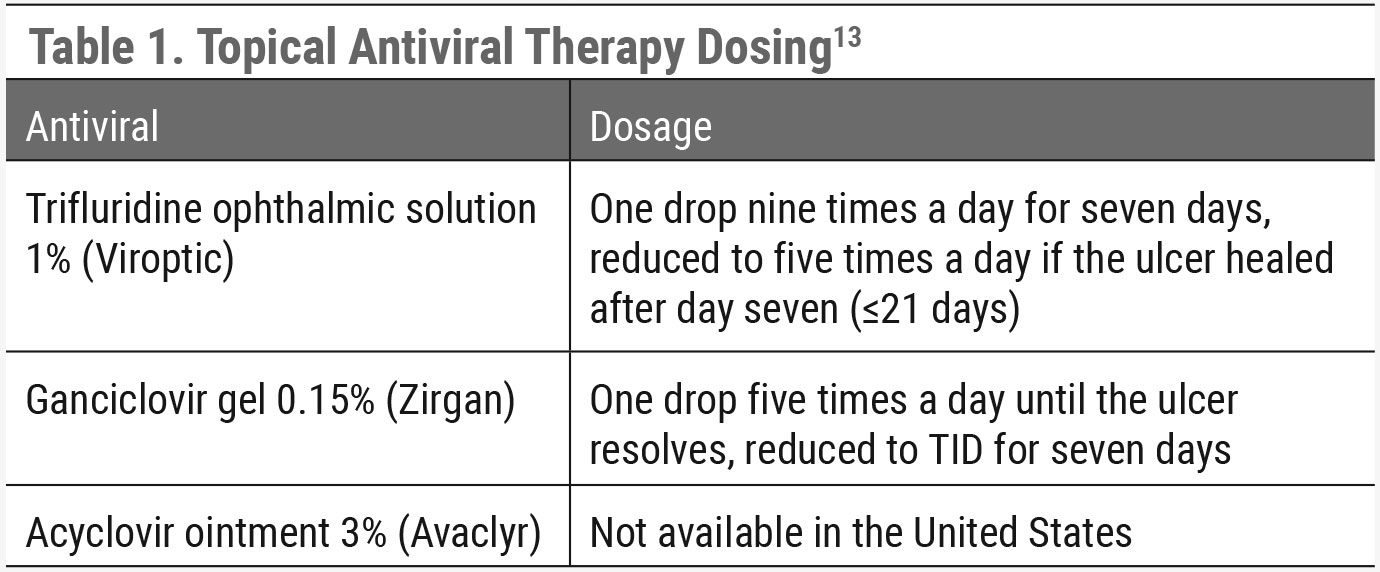 |
| Click table to enlarge. |
Clinical Presentations
HSVK can present with different corneal manifestations depending on what layer of the cornea the virus raids: the epithelium, stroma and/or endothelium.1 Herpes simplex epithelial keratitis is the most common subtype of HSVK and is responsible for 50% to 80% of all ocular herpes infections.14 Within 12 to 24 hours, infected epithelial cells form punctate vesicles. These vesicles, the beginning stages of dendrites, are formed by the swollen cell nuclei filled with replicating DNA viral load.5,15 As epithelial cells swell, apoptose and shed the virus, adjacent cells become infiltrated, ultimately causing a corneal dendrite.
These dendritic lesions present with granular epithelium, branching linear pattern, terminal bulbs and raised gray edges.5,16 The body of the dendrite stains with fluorescein dye while the borders of the terminal bulbs stain with rose bengal or lissamine green. The dendritic lesion may progress and form a geographic ulcer in 25% of cases.5 HSV epithelial keratitis is classically the most painful type of HSVK as epithelial cells are invaded by the herpes virus, causing epithelial cell death. Common symptoms include pain, tearing, photophobia, foreign body sensation, conjunctival injection and decreased vision.15 HSV stromal keratitis has two subtypes: HSV stromal keratitis with epithelial ulceration (necrotizing) and HSV stromal keratitis without epithelial ulceration (non-necrotizing). Meanwhile, HSV endothelial keratitis can be described as diffuse, linear or disciform.5.16
Herpes simplex stromal keratitis is considered an immune-mediated inflammatory response caused by viral antigens in the stroma. HSV stromal keratitis can present with or without epithelial ulceration. Herpes simplex stromal keratitis with ulceration is a rare form of HSV keratitis likely caused by live virus proliferation in the stroma.10 It presents as a gray-white opaque stromal edema with necrosis and ulceration of the overlying corneal epithelium.5 HSV stromal keratitis with ulceration is commonly misdiagnosed as bacterial keratitis due to its clinical presentation of an epithelial defect with a stromal infiltrate. Corneal neovascularization can originate from the periphery and encroach toward the inflammatory site of the stroma. If left untreated, HSV stromal keratitis can develop corneal thinning, ulceration and conclusive perforation.17 Other complications include the formation of a corneal abscess, keratic precipitates, anterior uveitis and elevated intraocular pressure (IOP).5
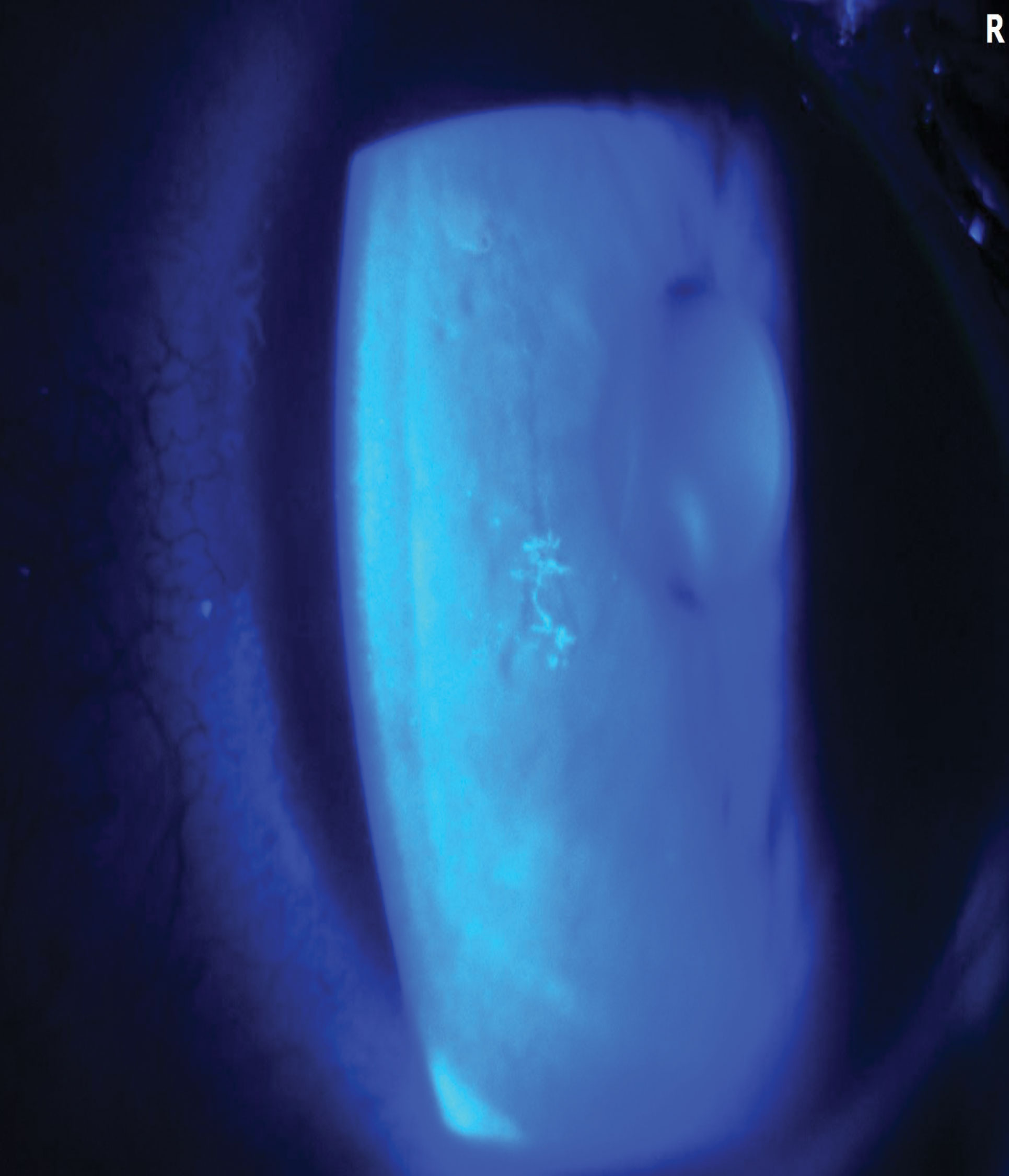 |
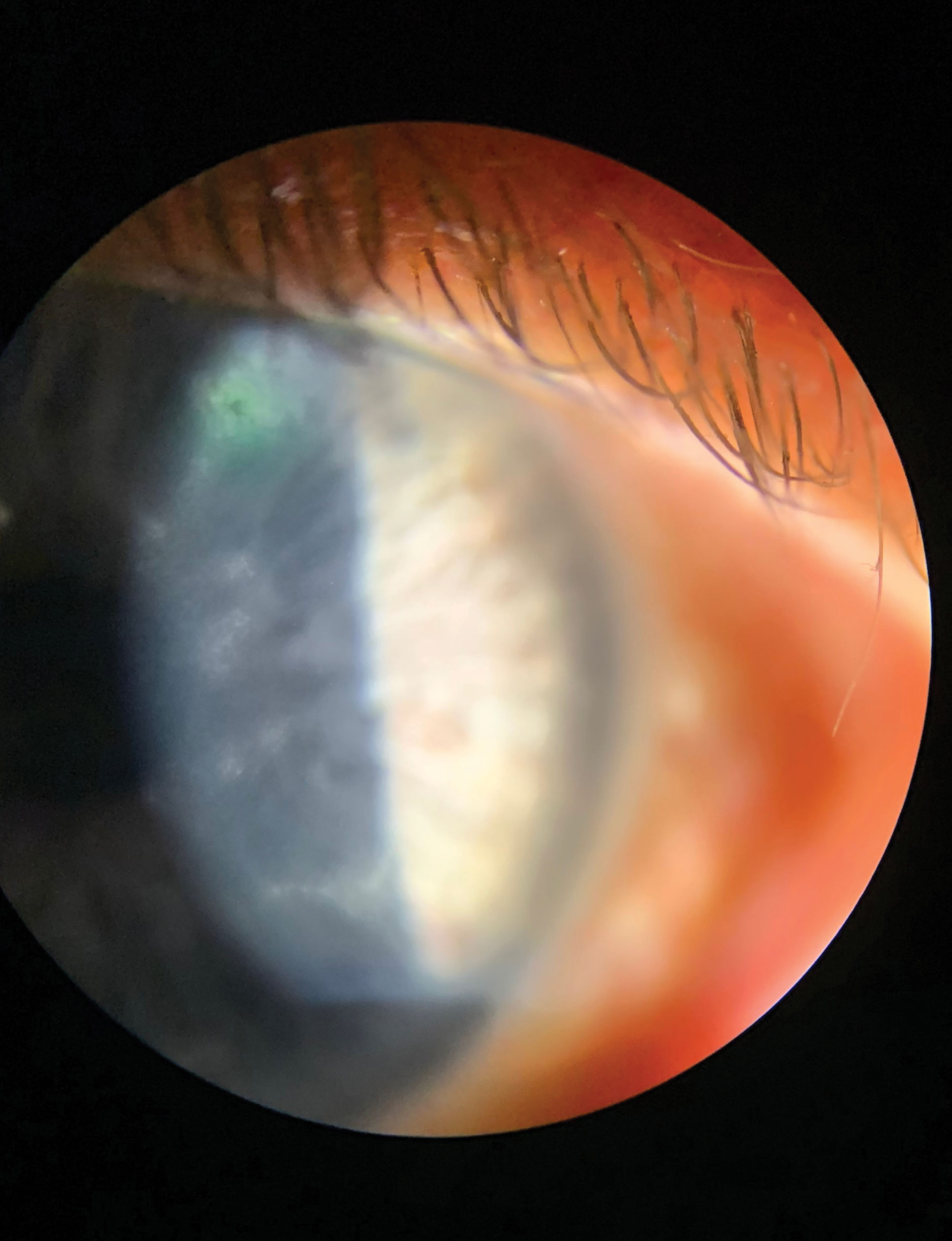
| Even patients who only demonstrate small dendrites such as this one can present with significant pain and discomfort. Click image to enlarge. |
Common symptoms for both HSV stromal keratitis with or without ulceration include photophobia, blurred vision, redness, photophobia and tearing.17 HSV stromal keratitis without ulceration is the most common form of HSV stromal keratitis. This subtype is sometimes referred to as “immune-mediated” or “non-necrotizing” and can be recurrent. It is caused by an inflammatory response against retained HSV antigens from a previous HSVK episode inducing an antibody-complement cascade in the stroma.5,10 This stromal inflammatory response can occur in the latent or active stages of the infection.6 Herpes simplex stromal keratitis without epithelial ulceration presents as a stromal infiltrate without any epithelial disruption. The stromal inflammation may be focal, multifocal, diffuse and/or associated with anterior uveitis. If chronic, it can cause neovascularization, corneal scarring and corneal thinning.5
HSV endothelial keratitis is another form of an immune-mediated response where the herpes virus spreads to the endothelium, causing endothelial cell dysfunction.14 Unlike HSV stromal keratitis, about half of these cases have no prior history of HSV epithelial keratitis and can occur independently from other forms of HSVK. HSV endothelial keratitis is commonly referred to as disciform keratitis; contrastingly, disciform is not completely accurate as HSV endothelial keratitis can also be considered linear or diffuse. The orientation of the associated keratic precipitates built up on the posterior wall of the endothelium and the extent of the stromal edema determines its classification.14 Disciform keratitis is the most common presentation of HSV endothelial keratitis, with disc-shaped stromal edema with underlying semi-circle-shaped keratic precipitates.5,16
Like the names suggest, linear endothelial HSVK has a vertical lined pattern of keratic precipitates and diffuse endothelial HSVK has keratic percipitates diffusely scattered across the entirety of the cornea. Clinical features of HSV endothelial keratitis include stromal edema caused by stromal deturgescence, overlying epithelial edema, inflammation of the endothelium with underlying keratic precipitates without significant anterior uveitis and elevated IOP.13 Common symptoms are pain, redness, tearing, blurred vision and photophobia. Recurrent endothelial keratitis can cause endothelial cell loss, chronic corneal edema, scarring, corneal structural damage and irregular astigmatism.1
Differential Diagnosis
One of the most difficult aspects of diagnosing and managing patients with HSVK is its wide variety of clinical manifestations. Due to its prevalence, consider HSVK as a possible diagnosis in any patient who presents with a unilateral red eye, especially with staining on the cornea. Familiarizing yourself with the differentials that may exhibit similar characteristics to HSVK will help to prevent delay in diagnosis and initiation of treatment.
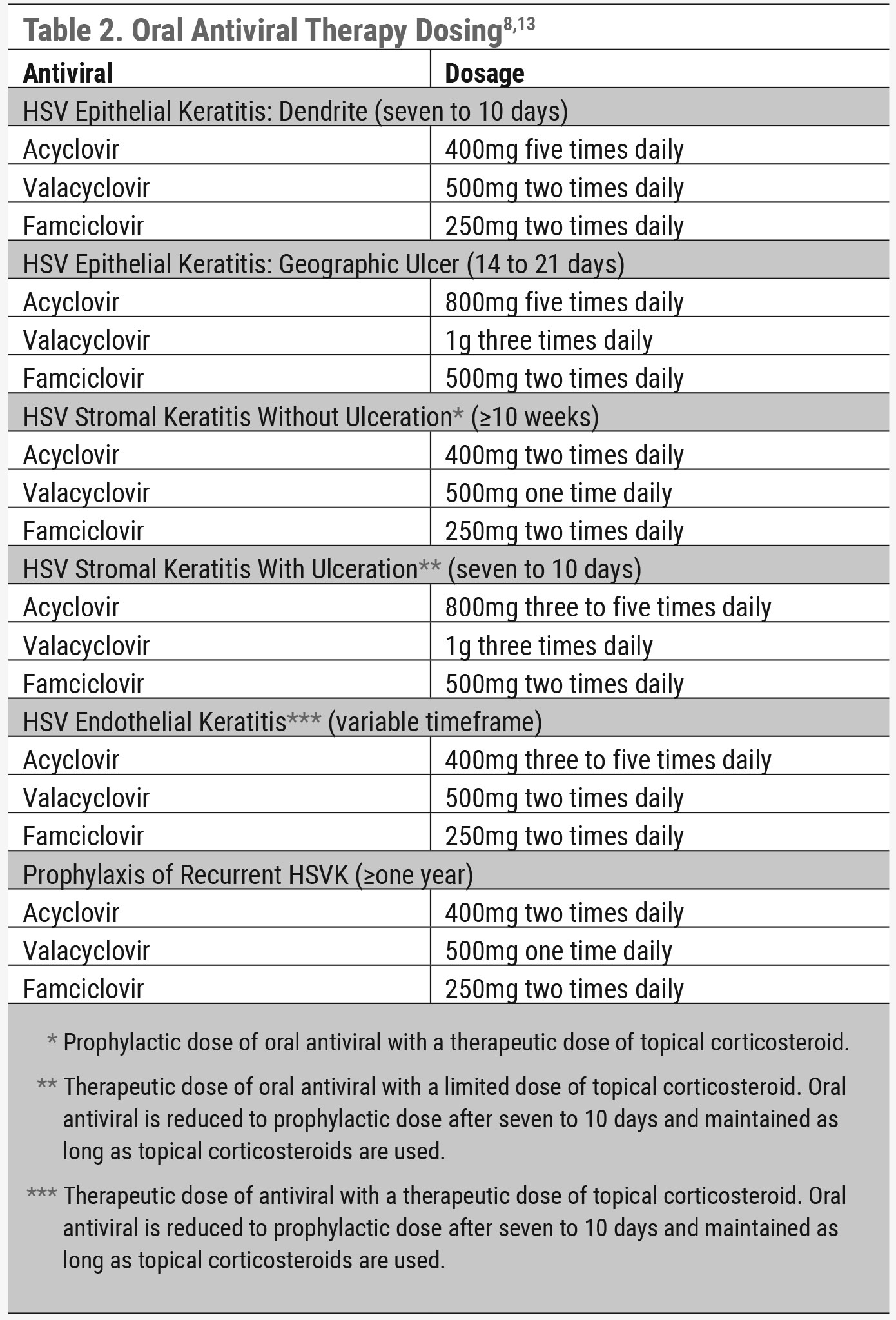 |
| Click table to enlarge. |
Due to the fact that HSVK can impact multiple layers of the cornea, the differentials may vary based on which layer of tissue is impacted. For example, dendritic epithelial keratitis may have different differentials than those of stromal or endothelial keratitis, although in some cases these may overlap. HSV epithelial keratitis differentials should include other types of infectious and noninfectious keratitis that may cause dendrite-like or geographic-like lesions on the cornea. This list may be extensive and should include varicella zoster viral keratitis, Acanthamoeba keratitis, microbial keratitis without stromal involvement (i.e., bacterial/fungal), Chlamydial epithelial keratitis, Epstein-Barr epithelial keratitis, recurrent corneal erosions, exposure keratopathy, Thygeson’s superficial punctate keratitis and epithelial basement membrane dystrophy (EBMD).13
Many of these conditions, such as Acanthamoeba keratitis and microbial keratitis, may be difficult to distinguish due to dendrite-like corneal presentations. Many times, these conditions can be differentiated based on a thorough clinical history. Acanthamoeba and bacterial keratitis are commonly associated with contact lens wear and water exposure. Fungal keratitis is likely associated with corneal insult or injury due to vegetation. HSVK can occur without contact lens use, water exposure or vegetative trauma. Other conditions such as Thygeson’s and EBMD differ from HSVK in that they most commonly present bilaterally, whereas bilateral HSVK is very rare.
Apart from HSV epithelial keratitis, HSV stromal and endothelial keratitis have their own list of differentials to consider. These separate conditions can also present with interstitial keratitis and keratouveitis that mimic the presentation of HSV stromal and endothelial disease.13 These differentials may include microbial keratitis with stromal involvement (any type), syphilis, Cogan’s syndrome, measles keratitis, mumps keratitis, Lyme disease, Posner-Schlossman syndrome, cytomegalovirus endothelial keratitis and corneal graft rejection.13
In many cases of HSVK differentials, possible diagnoses may be eliminated based on a thorough case history and clinical discussion with the patient. However, in cases where the puzzle cannot be solved based on verbal communication alone, use of corneal staining or, in some cases, laboratory testing may be needed to diagnose HSVK with confidence.
Treatment and Management
Complicating the proper diagnosis and treatment of HSV are the multiple corneal layers affected. The indicated medications and their dosages vary depending on the subtype of HSVK present. Treatment for HSVK includes oral antivirals, topical antivirals and topical corticosteroids; however, not all available treatment options are appropriate for each HSVK subtype. Thus, it is important to correctly diagnose the subtype of HSVK to formulate an appropriate treatment plan.
 |
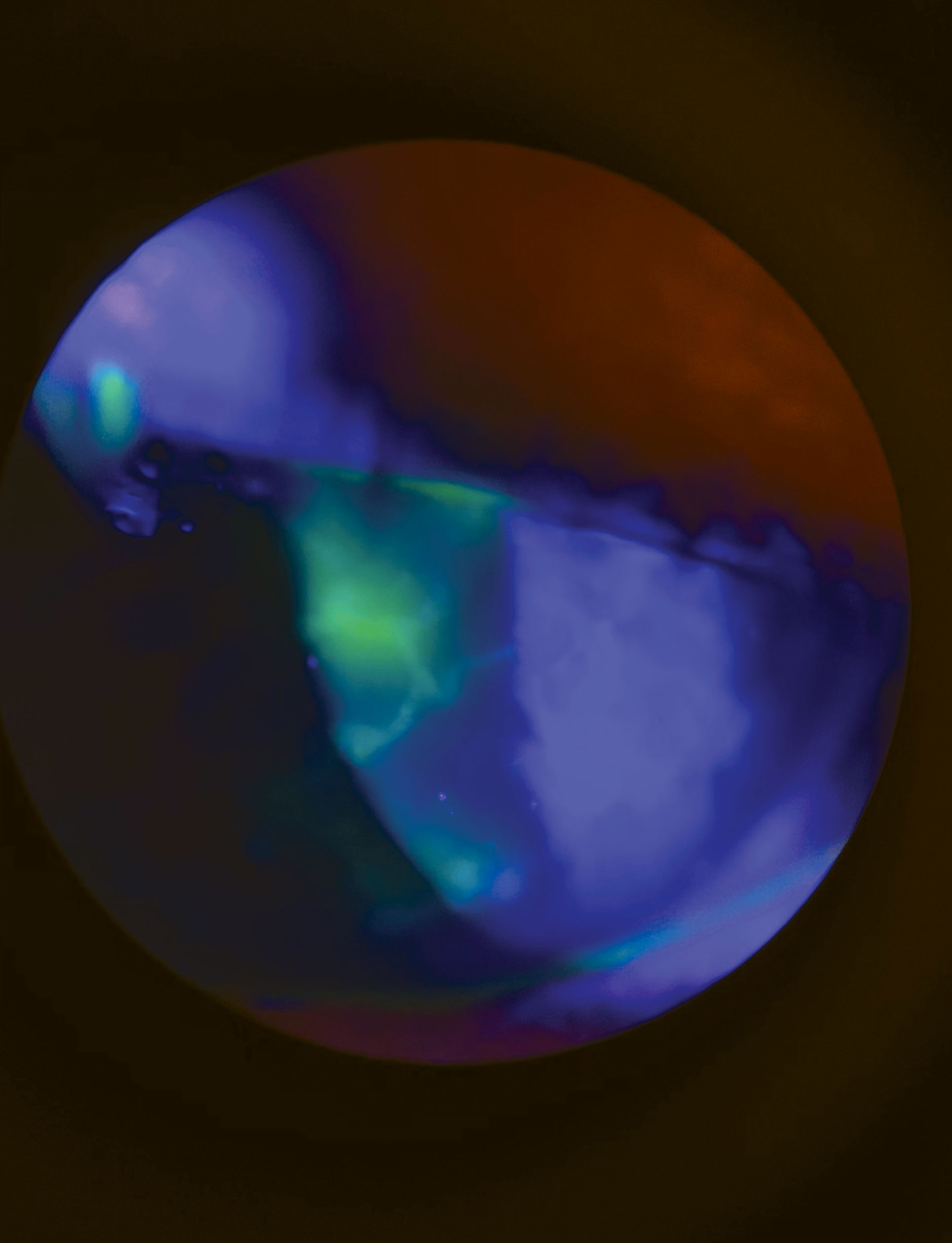
| A resolving central dendrite with multifocal stromal keratitis with ulceration in a patient with an aggressive form of ocular HSVK who is recovering from COVID-19. Click image to enlarge. |
There are three topical antivirals approved by the FDA as treatment for HSVK: trifluridine ophthalmic solution 1%, ganciclovir gel 0.15% and acyclovir ointment 3% (Table 1).13 Acyclovir ointment 3% is currently not available to be prescribed as it is still on the discontinued drug product list for reasons other than safety and effectiveness.18 Trifluridine ophthalmic solution 1% is known to be more toxic to the ocular surface than ganciclovir gel 0.15% since it is nonselective against DNA synthesis of both normal and viral-infected cells.5 The cellular and ocular surface toxicity caused by trifluridine ophthalmic solution 1% can result in epithelial keratitis and delayed reepithelization. In contrast, ganciclovir gel 0.15% does not target the DNA of healthy cells, thus causing less ocular surface toxicity.
Oral antiviral agents are considered off-label for the treatment of HSVK. Currently, the available oral antivirals are acyclovir, valacyclovir and famciclovir (Table 2).8,13 These oral antiviral agents have excellent corneal and anterior chamber penetrance making them effective treatment options for HSVK. However, due to the possibility of renal injury caused by oral antiviral agents, there needs to be special consideration when prescribing them for patients with kidney disease as there can be issues with the metabolism and excretion of the medication.8
HSV epithelial keratitis. Oral antiviral agents are commonly used as treatment for HSVK epithelial keratitis without the use of topical corticosteroids, which are contraindicated as they can prolong epithelialization and cause the dendrite to progress into a geographic ulcer.16 The benefits of treating with oral antivirals instead of topical antivirals are that they are more affordable, have reduced dosing schedules and are not toxic to the cornea. Both topical and oral antivirals have independently been shown to be equally effective in treating HSV epithelial keratitis; however, there has not been sufficient evidence that treating HSV keratitis with both oral and topical antivirals hastens the healing process.5,16
The HEDS study showed no added benefit in concurrently treating HSVK with topical and oral antivirals.13 For HSV epithelial keratitis, oral acyclovir is dosed 400mg five times a day for seven to 10 days, valacyclovir is dosed 500mg two times a day for seven to 10 days and famciclovir is dosed 250mg two times a day for seven to 10 days.6,13 If treating with topical antivirals, trifluridine ophthalmic solution 1% is dosed one drop nine times a day for seven days and then reduced to five times a day if the ulcer has healed after day seven. Treatment with trifluridine ophthalmic solution 1% should not exceed 21 days due to the associated risk of ocular toxicity. Ganciclovir gel 0.15% is dosed one drop five times a day until the ulcer resolves and then reduced to three times a day for seven days.13 For geographic ulcers, the dosages for oral antivirals are doubled for a treatment period of 15 to 21 days.
HSV stromal keratitis without ulceration. HSV stromal keratitis is considered an immune-mediated response to viral antigens in the stroma. Thus, a therapeutic dose of topical corticosteroids is needed to quell the inflammatory response alongside a dose of oral antivirals. It is important that oral antivirals are used while the patient is being treated with topical corticosteroids. In HSV stromal keratitis without ulceration, oral acyclovir is dosed 400mg twice daily, valacyclovir is dosed 500mg once daily and famciclovir is dosed 250mg twice daily. Topical corticosteroids can be dosed six to eight times daily and should be used for at least 10 weeks and tapered slowly as the cornea improves. Developing a treatment plan for HSVK is more of an art than a science, as the treatment is based on the patient’s medical and ocular history, clinical presentation and rate of healing. Also, considering HSV stromal and endothelial keratitis are unpredictable in nature with the risk of permanent vision loss, refer these patients to a board-certified corneal specialist to help with comanagement.
 |
| A corneal dendrite can be large and cause severe pain and discomfort. Click image to enlarge. |
HSV stromal keratitis with ulceration. When ulceration is present, the treatment plan needs to change. A limited dose of topical corticosteroids can be used along with a therapeutic dose of an oral antiviral. Oral acyclovir is dosed 800mg three to five times a day for seven to 10 days, valacyclovir is dosed 1g three times a day for seven to 10 days and famciclovir is dosed 500mg two times a day for seven to 10 days. The oral antiviral should then be reduced to a prophylactic dose and maintained throughout the duration of treatment with the topical corticosteroid. There is a lack of data that supports any specific recommended length of treatment for this subtype of HSVK; therefore, clinical experience and presentation greatly aid in developing the treatment plan.13 Again, patients with HSV stromal keratitis should be further managed by a board-certified corneal specialist. Oral antivirals are preferred in treating any form of HSV stromal keratitis or endothelial keratitis since trifluridine ophthalmic solution 1% and ganciclovir gel 0.15% do not have adequate corneal stroma penetration.13
HSV endothelial keratitis. This is relatively uncommon, and there are only a few studies that provide recommended treatment plans. Treatment with topical corticosteroids is needed, since it is an inflammatory-mediated response to the virus in the corneal endothelium. HSV endothelial keratitis responds extremely well to topical corticosteroids and, in comparison to HSV stromal keratitis, HSV endothelial keratitis heals at a remarkably faster rate.8,13 Therapeutic doses of both topical corticosteroids and oral antiviral agents are needed for this subtype of HSVK. Topical corticosteroids can be dosed one drop six to eight times a day and tapered slowly. Oral acyclovir is dosed 400mg three to five times daily, valacyclovir is dosed 500mg two times daily and famciclovir is dosed 250mg two times daily. The therapeutic dose of oral antiviral should be reduced to seven to 10 days and maintained throughout the entire course of the topical corticosteroid taper schedule. Ganciclovir gel 0.15% and trifluridine ophthalmic solution 1% are not recommended in treating HSV endothelial keratitis due to their poor corneal penetrance.13 Given the challenging nature of this condition, comanagement with a specialist can be useful for both the optometrist and their patient.
Life After HSVK
A previous history of HSV stromal keratitis and recurrent HSVK increases the risk of future HSVK recurrence.13 An oral antiviral maintenance dose can be introduced for patients who are at a higher risk to prevent recurrence of HSVK. The HEDS II study found a 45% reduction in recurrent episodes of ocular HSVK when on prophylactic treatment.19 The maintenance dose for acyclovir 400mg is two times daily for one year, valacyclovir 500mg is one time daily for one year and famciclovir is two times daily for one year.
 |
| HSV stromal keratitis with or without ulceration can be focal, multifocal or diffuse. This patient has HSV stromal keratitis with epithelial involvement. Click image to enlarge. |
This long-term maintenance dose can be extended past one year for special cases that present a higher risk of recurrence, such as in immunocompromised patients. As for prophylaxis, a patient with a history of HSVK may also be on a short-term maintenance dose if they plan to undergo any ocular surgeries such as cataract surgery. Lastly, an oral antiviral maintenance dose is needed if a patient were to be prescribed a corticosteroid at any time.
HSV stromal keratitis and endothelial keratitis, whether initial or recurrent episodes, are the greatest threat to permanent corneal structural damage and vision loss. These inflammatory reactions can cause corneal scarring, neovascularization, corneal thinning, decreased corneal sensation and fibrosis. Recurrent episodes place the patient at a higher risk of developing permanent corneal structural abnormalities. Approximately one million people worldwide are affected by permanent visual impairment due to ocular HSV.13 There are also a reported 1,000 penetrating keratoplasties annually in the United States due to visually significant corneal scarring from ocular HSV.13
It is imperative to be vigilant in recognizing early clinical signs and symptoms of HSVK to help prevent severe cases from causing visually significant corneal damage. It is also important to educate patients and discuss possible visual outcomes and options. Comanaging with a corneal specialist is crucial in reducing your liability as a provider.
Depending on the course of the condition, the patient may benefit from an amniotic membrane for improved epithelial healing or a specialty contact lens for improved vision. A patient with significant corneal scarring and decreased vision may experience an improvement in vision from specialty lenses such as scleral lenses.
HSVK is a common and often visually devastating condition. Doctors of optometry can better manage these patients through a detailed understanding of the clinical presentation, differentials and treatments. This not only increases confidence in managing the condition but also improves outcomes and overall visual prognosis.
Drs. Martinez and Leon practice at the South Texas Eye Institute in San Antonio, TX. They are graduates of the Rosenberg School of Optometry, where they completed their optometry degrees and residencies in primary care. They have no financial interests to disclose.
1. Azher TN, Yin XT, Tajfirouz D, et al. Herpes simplex keratitis: challenges in diagnosis and clinical management. Clin Ophthalmol. 2017;11:185-91. 2. Whitley RJ. Herpesviruses. In: Baron S, editor. Medical Microbiology. 4th edition. Galveston (TX): University of Texas Medical Branch at Galveston; 1996. Chapter 68. Available from: https://www.ncbi.nlm.nih.gov/books/NBK8157/. 3. Ahmad B, Patel BC. Herpes Simplex Keratitis. [Updated 2021 Nov 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK545278/. 4. Sibley D, Larkin DFP. Update on Herpes simplex keratitis management. Eye (Lond). 2020;34(12):2219-26. 5. Tsatsos M, MacGregor C, Athanasiadis I, et al. Herpes simplex virus keratitis: an update of the pathogenesis and current treatment with oral and topical antiviral agents. Clin Exp Ophthalmol. 2016;44(9):824-37. 6. Leon, S. Herpes Simplex Keratitis: Managing the Masquerader. Review of Cornea and Contact Lenses. 2020. 7. Chan RVP (Ed.). Herpes simplex keratitis - Europe. American Academy of Ophthalmology. 2013. https://www.aao.org/topic-detail/herpes-simplex-keratitis--europe. 8. Leon S. Be a Hero to Your HSVK Patients. Review of Optometry. 2017. https://www.reviewofoptometry.com/article/ro0717-be-a-hero-to-your-hsvk-patients2. 9. Chodosh J, Ung L. Adoption of Innovation in Herpes Simplex Virus Keratitis. Cornea. 2020;39(1):S7-S18. 10. Welder JD, Wagoner MD, Kitzmann AS. Herpes Simplex Keratitis. EyeRounds.org. 2012. https://eyerounds.org/cases/160-HSV.htm. 11. American Academy of Ophthalmology. Herpes Zoster Ophthalmicus. https://www.aao.org/focalpointssnippetdetail.aspx?id=8367b620-245c-4ebf-89e7-eca0c8d35aa3. 12. Bronner A. Get to Know HZO. Review of Optometry Continued Education. 2021. https://www.revieweducationgroup.com/ce/get-to-know-hzo. 13. White ML, Chodosh J. Herpes simplex virus keratitis: a treatment guideline. The American Academy of Ophthalmology Clinical Guidelines. June 2014. https://www.aao.org/clinical-statement/herpes-simplex-virus-keratitis-treatment-guideline. 14. Zhu L, Zhu H. Ocular herpes: The pathophysiology, management and treatment of Herpetic Eye Diseases. Virol Sin. 2014;29(6):327-42. 15. Roozbahani M, Hammersmith KM. Management of Herpes Simplex Virus Epithelial Keratitis. Curr Opin Ophthalmol. 2018;29(4):360-4. 16. Chodosh J, Ung L. Adoption of Innovation in Herpes Simplex Virus Keratitis. Cornea. 2020;39(1):S7-S18. 17. Wang L, Wang R, Xu C, et al. (2020). Pathogenesis of Herpes Stromal keratitis: Immune Inflammatory Response Mediated by Inflammatory Regulators. Front Immunol. 2020;11:766. 18. Roth L. Determination That AVACLYR (Acyclovir Ophthalmic Ointment), 3 Percent, Was Not Withdrawn From Sale for Reasons of Safety or Effectiveness. Federal Register. 2021. https://www.federalregister.gov/documents/2021/05/20/2021-10593/determination-that-avaclyr-acyclovir-ophthalmic-ointment-3-percent-was-not-withdrawn-from-sale-for. 19. Austin A, Lietman T, Rose-Nussbaumer J. Update on the Management of Infectious Keratitis. Ophthalmology. 2017;124(11):1678-89. |
