 |
Ocular Side Effects of New Cancer Agents
Understanding how molecularly targeted chemotherapeutic agents can impact patients is key for primary eyecare providers.
By Julia Canestraro, OD
Release Date: March 15, 2023
Expiration Date: March 15, 2026
Estimated Time to Complete Activity: 2 hours
Jointly provided by Postgraduate Institute for Medicine (PIM) and Review Education Group
Educational Objectives: After completing this activity, the participant should be better able to:
Recognize the potential ocular side effects of targeted cancer therapies.
Monitor patients on these drugs for potential ocular adverse events.
Comanage these patients with specialists when needed.
Educate their patients on how these medications may impact their eye health.
Target Audience: This activity is intended for optometrists engaged in cancer patient management.
Accreditation Statement: In support of improving patient care, this activity has been planned and implemented by PIM and the Review Education Group. PIM is jointly accredited by the Accreditation Council for Continuing Medical Education, the Accreditation Council for Pharmacy Education and the American Nurses Credentialing Center to provide CE for the healthcare team. PIM is accredited by COPE to provide CE to optometrists.
Reviewed by: Salus University, Elkins Park, PA
Faculty/Editorial Board: Julia Canestraro, OD
Credit Statement: This course is COPE approved for 2 hours of CE credit. Activity #125569 and course ID 83324-PH. Check with your local state licensing board to see if this counts toward your CE requirement for relicensure.
Disclosure Statements: PIM requires faculty, planners and others in control of educational content to disclose all their financial relationships with ineligible companies. All identified conflicts of interest are thoroughly vetted and mitigated according to PIM policy. PIM is committed to providing its learners with high-quality, accredited CE activities and related materials that promote improvements or quality in healthcare and not a specific proprietary business interest of an ineligible company.
Those involved reported the following relevant financial relationships with ineligible entities related to the educational content of this CE activity: Author: Dr. Canestraro has no relevant financial interests to disclose. Managers and Editorial Staff: The PIM planners and managers have nothing to disclose. The Review Education Group planners, managers and editorial staff have nothing to disclose.
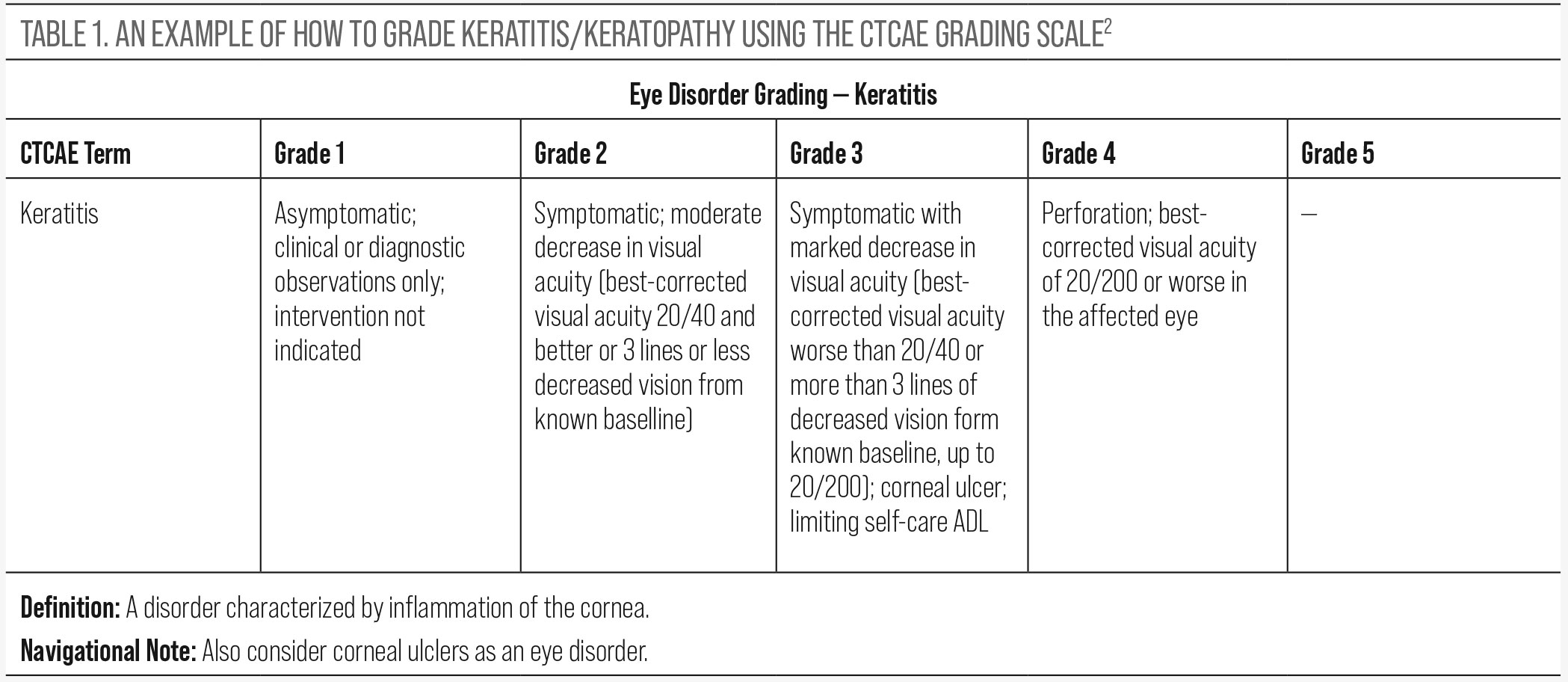 |
| Click table to enlarge. |
The Centers for Disease Control and Prevention reported approximately 1.7 million new invasive cancer cases in the United States in 2019.1 As primary eyecare providers, we will encounter patients undergoing cancer treatment who may have ocular sequelae as a result.
Traditional chemotherapeutic agents can cause a variety of side effects that may affect all ocular tissue ranging from dry eye to optic neuropathy. However, the face of cancer treatment is shifting toward specialized treatment, targeting specific pathways for certain types of cancers, and with this shift comes a range of different ocular toxicities. And so, primary eyecare providers need to be familiar with newer cancer drugs and the possible ocular sequelae of these agents.
In this article, we will discuss molecularly targeted agents and the ones most likely to cause ocular toxicity. This is not an exhaustive list but offers optometrists insight into some of the most common agents they may see in their clinical practice and how to provide comprehensive care to their patients.
Introduction to Grading Ocular Toxicity
Ocular toxicity is graded using the Common Terminology in Cancer Adverse Events (CTCAE v5.0) grading scale.2 The grading scale was created to allow for common labelling and grading of drug toxicity in various parts of the body. Specifically for the eye, it provides guidelines for grading various eye disorders such as blurred vision, dry eye, keratitis, uveitis and retinopathy, to name a few, and allows for accurate reporting of side effects. This grading scale should be used as a reference when grading ocular toxicity and can be easily found online (Table 1). It is worth mentioning that some drug companies manufacturing antibody drug conjugates (i.e., Elahere) have created their own keratopathy grading scale, and this can be used as a guideline instead.
Antibody Drug Conjugates (ADCs)
This increasingly used targeted cancer therapy is comprised of a tumor-specific monoclonal antibody with a potent anti-cancer agent through a chemical linker.3 Targeted malignancies include ovarian cancer, cervical cancer, B-cell lymphoma, multiple myeloma, breast cancer, urothelial cancer and leukemia.3 There are currently 11 FDA-approved ADCs including Kadcyla (ado-trastuzumab emtansine), Enhertu (fam-trastuzumab deruxtecan-nxki), Tivdak (tisotumab vedotin-tftv) and Elahere (mirvetuximab soravtansine-gynx). The other FDA-approved ADCs (which will not be discussed in this article) are Mylotarg (gemtuzumab ozogamicin), Adcetris (brentuximab vedotin), Besponsa (inotuzumab ozogamicin), Poliyv (polatuzumab vedotin-piiq), Padcev (enfortuamb vedotin-ejfv), Trodelvy (sacituzumab govitecan-hziy) and Zynlonta (locastuximab tesirine-lpyl).
Toxicity. The incidence of corneal toxicity (often referred to as keratopathy) ranges from 11% to 37% in clinical trials, depending on the ADC.4,5 In clinical trials, 3.2% of patients on Tivdak developed severe ulcerative keratitis and 40% experienced conjunctival adverse reactions, including conjunctivitis, conjunctival abrasion and conjunctival hyperemia.6 Elahere caused uveitis in 1% of patients.5
Microcyst-like epithelial changes (MECs) develop in the epithelial layer of the cornea. These spherical “cysts” do not stain with fluorescein dye and are best visualized with a parallelopiped slit lamp beam or indirect illumination (Figure 1). Ocular dryness with resulting corneal staining and refractive error changes can occur. Hyperopic shifts are seen in early treatment while myopic changes are more common in later treatment.3 The resulting decreased vision from corneal staining and refractive shifts generally reverses with cessation of the drug. The mechanism for what causes corneal MECs is still not fully understood, but the most recent literature suggests that the ADC enters the corneal epithelial cells, the cells become apoptotic (observed as MECs) and these cells are eventually shed and replaced by new epithelial cells.7
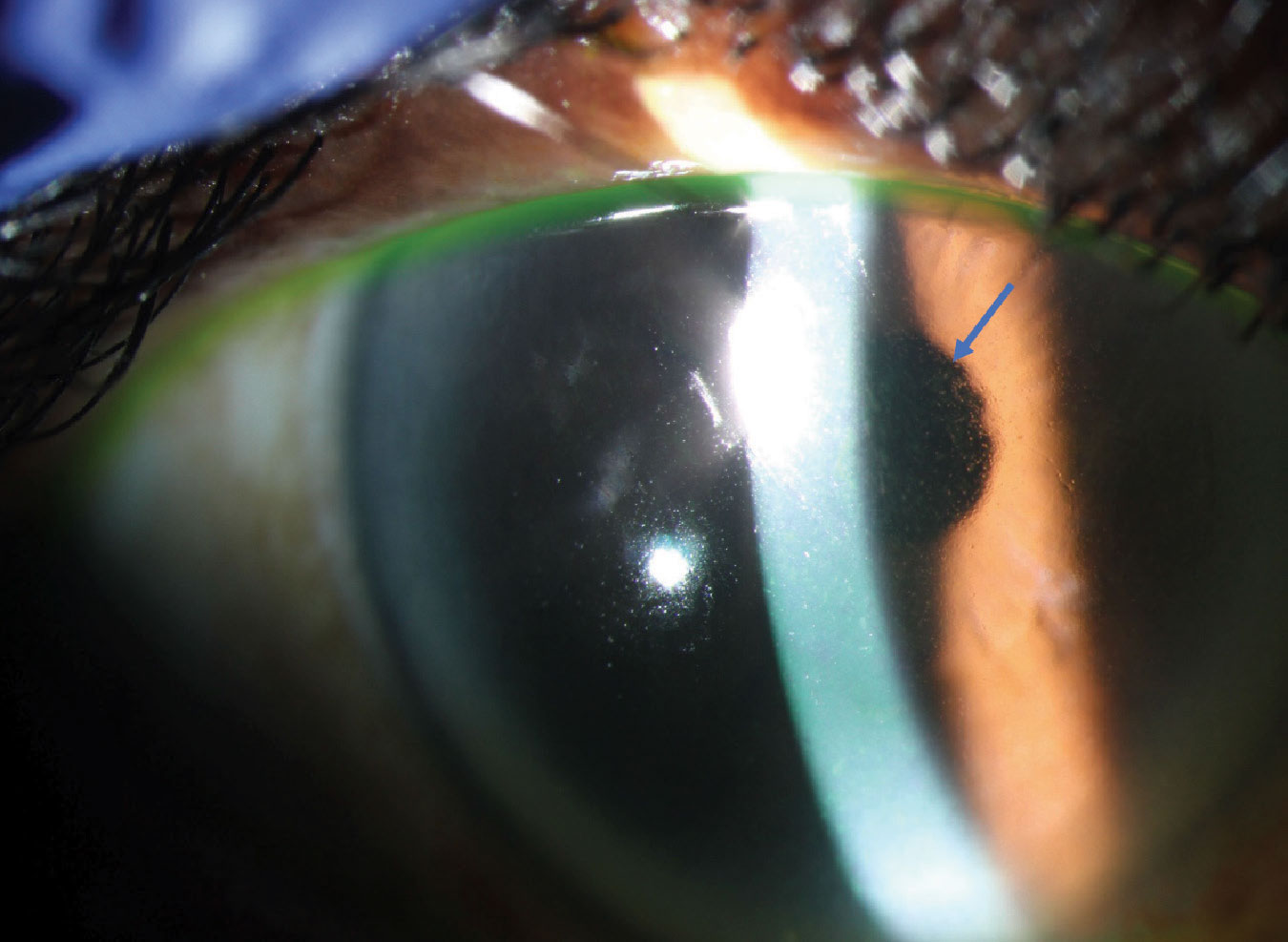 |
Fig. 1. Corneal MECs (blue arrow) in a patient with ADC-related keratopathy. Click image to enlarge. |
Treatment and management. There is no treatment for MECs, and they are often observed if there is no change in vision. If and when the cancer treatment is discontinued, the MECs will resolve within weeks to months. Treatment of concomitant dry eye includes preservative-free artificial tears at least three times a day and cyclosporine ophthalmic solution or emulsion, or lifitegrast ophthalmic solution, if needed. Treating concomitant blepharitis with lid hygiene and/or warm compresses is also recommended. Treatment of uveitis or conjunctivitis includes corticosteroid drops. The use of contact lenses is restricted in these patients, as there is a concern for the drug sitting in the tear film and therefore absorbing into the contact lens and exacerbating keratopathy, although this has not been formally studied to date. If vision is severely impacted with/without moderate to severe keratopathy, the drug may be held or given at a lower dose, as deemed by the oncologist.
A baseline eye exam is critical to ensure the cornea is healthy and to make note of any other ocular pathology. Patients should be educated thoroughly on possible ocular side effects, including blurred vision and dry eye, prior to starting treatment so they can expect the changes that may come. It is worth mentioning that these changes to the cornea are generally reversible and rarely cause permanent changes in vision.
Both Tivdak and Elahere have an FDA black box warning and therefore require ocular toxicity monitoring at baseline and prior to each dose for Tivdak and every other cycle for the first eight cycles for Elahere. Patients on Tivdak are required to instill vasoconstricting eye drops the day of infusion and corticosteroid drops on days zero through four of each treatment cycle.6 Patients on Elahere are required to use corticosteroid drops before day one and through day eight of each treatment cycle.5 Results of the eye examination, including ocular toxicity grading, must be reported to the oncologist each visit (particularly for Elahere and Tivdak), as they determine whether the patient should proceed with treatment and may also impact dosing. Comanagement with ophthalmology may be needed for cases of severe keratopathy or corneal ulceration.
BRAF Inhibitors
These agents are approved for the treatment of BRAF v600E mutant melanoma.8 The mitogen-activated protein kinase (MAPK) signaling pathway regulates the proliferation of melanoma cells, and these drugs target BRAF kinase, which interferes with this MAPK pathway.8 BRAF inhibitors are now often prescribed in combination with MEK inhibitors, thereby increasing the probability of ocular toxicity. Examples of FDA-approved BRAF inhibitors include Zelboraf (vemurafenib), Tafinlar and Rafinlar (dabrafenib) and Braftovi (encorafenib).
Toxicity. The most common ocular toxicities are dry eye/conjunctivitis, which occurred in approximately 2% of patients, and uveitis (ranging from anterior to posterior), which was observed in 4% to 9% of patients receiving Zelboraf.9,10 This agent may also cause cutaneous squamous cell carcinoma, verruca vulgaris lesions and keratoacanthoma, which can be found on the eyelid (Figure 2).
 |
Fig. 2. Eyelid verruca in a patient treated with a BRAF Inhibitor.10 Click image to enlarge. |
Treatment and management. Dry eye symptoms from BRAF inhibitors are generally mild and often do not require intervention or can be managed with artificial tears. Depending on the location of the uveitis, it can be treated with topical, periocular or intraocular corticosteroids, in addition to cessation, paused or continued drug therapy (at the same or a lower dose). Braftovi’s label specifies it should be withheld for a grade 1 or 2 uveitis that does not respond to ocular treatment, or for any grade 3 uveitis.
Squamoproliferative lesions (particularly squamous cell carcinoma) should be referred for surgical excision, and patients are often able to continue drug therapy. Braftovi’s label specifies that ophthalmologic evaluation should be performed at regular intervals and for any new or worsening disturbances. Clinically or visually significant findings, including ocular toxicity grading, must be reported to the oncologist as they may impact dosing and treatment, and comanagement with ophthalmology may be needed.
EGFR Inhibitors
Epidermal growth factor receptor (EGFR) is a glycoprotein that is abnormally activated in a variety of cancers, leading to cellular proliferation, differentiation and survival.12 EGFR inhibitors are used to target EGFR and treat metastatic colorectal cancer, head and neck cancer, non-small cell lung cancer, pancreatic cancer and some types of breast cancer. Current FDA-approved EGFR inhibitors include Erbitux (cetuximab), Vectibix (panitumumab) and Rybrevant (amivantamab). Examples of small molecule EGFR inhibitors are Tarceva (erlotinib), Iressa (gefitinib) and Exkivity (mobocertinib).
Toxicity. Dry eye is a common side effect of these drugs, due to poor healing of the corneal epithelium, and can lead to persistent epithelial defects.13 Other anterior segment findings include conjunctivitis, blepharitis and, very rarely, corneal thinning/melt.13 There are rare cases of anterior uveitis reported with Tarceva. All drugs in this class have been associated with hypertrichosis and trichomegaly, which in some case have caused corneal ulceration due to eyelashes misdirected at the cornea.14 Figure 3 demonstrates both blepharitis and trichomegaly in a patient treated with an EGFR inhibitor.
Treatment and management. Dry eye can be managed with lubricating drops and cyclosporine ophthalmic solution or emulsion, or lifitegrast ophthalmic solution, if needed. Blepharitis can be managed with lid hygiene, warm compresses and steroid/antibiotic ointments.13 These patients should be monitored routinely, particularly if symptoms develop. There is no set interval as indicated by the pharmaceutical companies for ocular toxicity monitoring of these drugs. Clinically or visually significant findings, including ocular toxicity grading, must be reported to the oncologist as they may impact dosing and treatment.
FGFR Inhibitors
Fibroblast growth factor receptor (FGFR) inhibition interferes with the MAPK signaling pathway, and the retina expresses targets of this pathway, thereby causing retinal toxicity.15 These drugs treat cancers such as FGFR-mutated urothelial cancer and cholangiocarcinoma. FDA-approved agents include Balversa (erdafitinib), Pemazyre (pemigatinib) and Truseltiq (infigratinib).
Toxicity. Patients may develop serous retinopathy and have similar characteristics to MEK inhibitor-associated retinopathy. OCT reveals fluid between the interdigitation zone and retinal pigment epithelium in varying configurations. Dry eye and trichomegaly are also reported side effects of these drugs.14
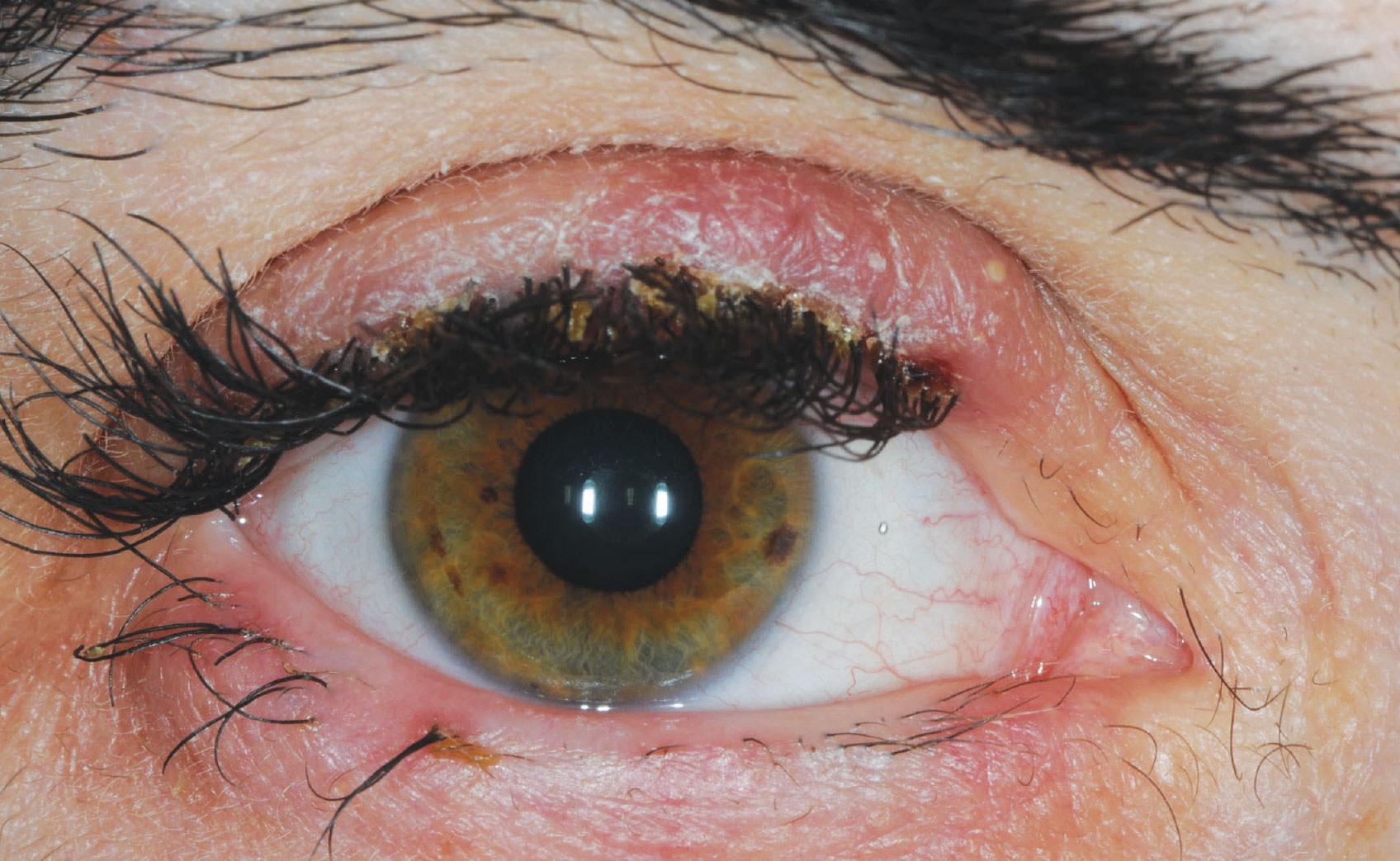 |
Fig. 3. Blepharitis and trichomegaly in a patient treated with an EGFR inhibitor. Click image to enlarge. |
Treatment and management. Patients taking Balversa should stop treatment if serous retinopathy occurs. It may be restarted if the fluid resolves within four weeks; otherwise the drug should be discontinued. It should also be discontinued in the scenario of grade 4 ocular toxicity.
Patients taking Pemazyre can be monitored on the drug if they are asymptomatic and if retinopathy is stable. If they are symptomatic or their retinopathy worsens, the agent should be held and re-examined. The patient may only resume the drug if symptoms and retinopathy improve.
Patients taking Truseltiq may continue at the same dose if retinopathy occurs; however, if it does not resolve within two weeks, the drug should be held until resolution of fluid. It can then be restarted at the same or a lower dose.
Patients on Balversa should be examined monthly during the first four months of treatment, then every three months thereafter. Patients taking Pemazyre should be examined at baseline, every two months for the first six months of treatment and then every three months thereafter. Patients taking Truseltiq should be monitored at baseline and then one month, three months and every three months thereafter during treatment.
All patients should be seen urgently for any visual symptoms, and examination should include visual acuity testing, slit lamp evaluation and OCT imaging. Clinically or visually significant findings, including ocular toxicity grading, must be reported to the oncologist as they may impact dosing and treatment, and comanagement with ophthalmology may be needed.
Immune Checkpoint Inhibitors (ICI)
This anti-cancer therapy is now widely used to treat advanced cancers. There are three main classes of checkpoint inhibitors, which act by potentiating the immune system to attack cancer cells. The classes include cytotoxic T-lymphocyte-associated antigen-4 (CTLA-4), programmed cell death (PD-1) and programmed cell death protein 1 (PD-L1) inhibitors. They have been approved by the FDA to treat various types of cancers such as melanoma, non-small cell lung cancer, renal-cell carcinoma, urothelial carcinoma and Hodgkin’s lymphoma.
By unleashing the immune system to attack cancer cells, ICIs can also cause an inflammatory reaction in healthy cells, thereby resulting in immune-related adverse events.16 There are a number of FDA-approved ICIs, including Yervoy (ipilimumab), Imjudo (tremelimumab), Keytruda (pembrolizumab), Opdivo (nivolumab), Libtayo (cemiplimab), Tecentriq (atezolizumab), Bavencio (avelumab) and Imfinzi (durvalumab).
Toxicity. Ocular immune-related adverse events occur in about 1% of patients. Inflammation of any part of the eye is possible with ICI treatment. Potential adverse events include blepharitis, conjunctivitis, keratitis, uveitis (anterior or posterior), vitritis, retinitis, orbital myositis (Graves’-like ophthalmopathy), cranial neuritis and optic neuritis.16
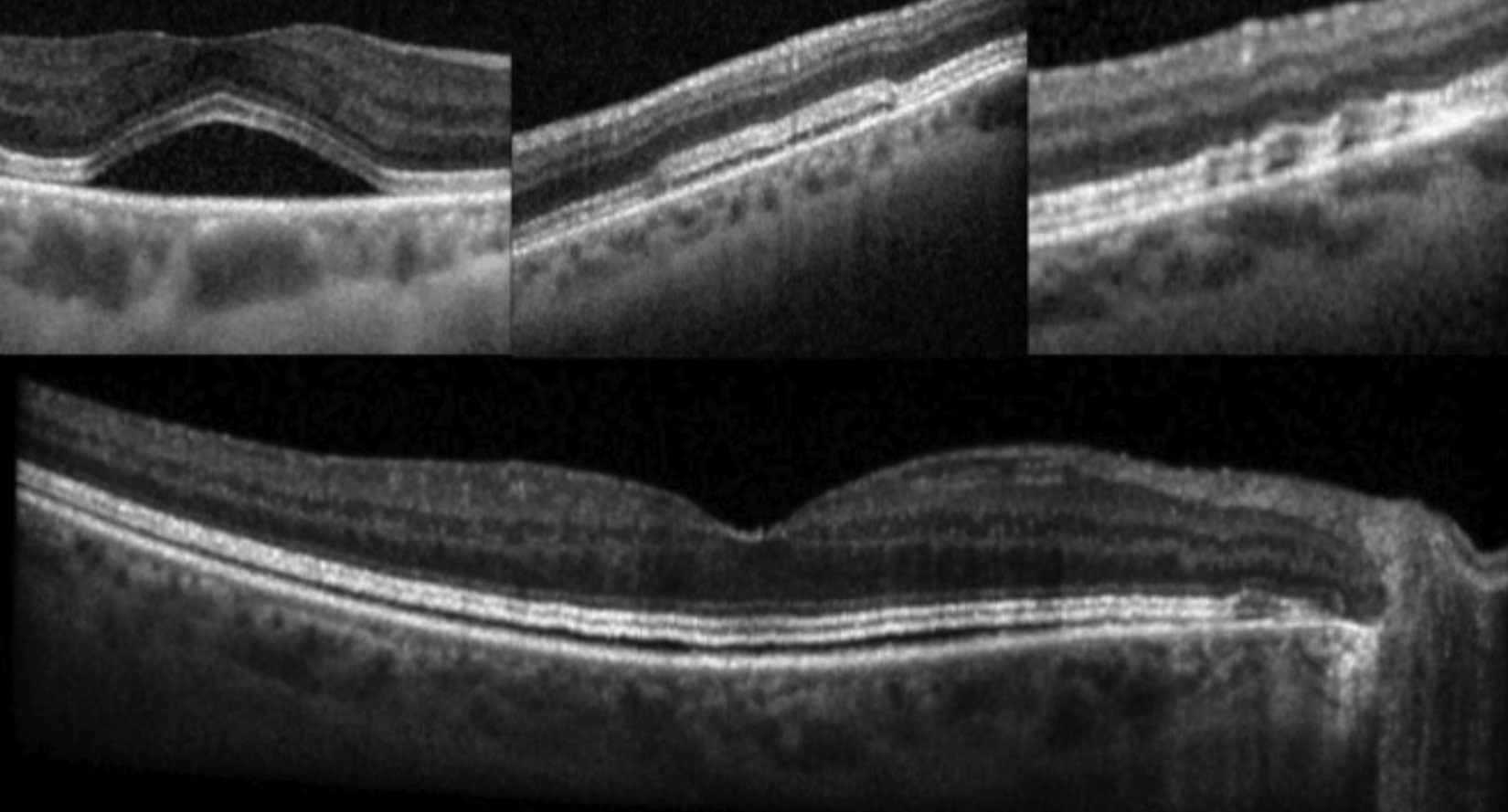 |
Fig. 4. OCT reveals fluid between the interdigitation zone and retinal pigment epithelium in varying configurations in patients with MEKAR.16 Click image to enlarge. |
Treatment and management. Treatment of anterior segment inflammation includes topical corticosteroid drops (i.e., prednisolone acetate ophthalmic suspension four times per day in both eyes). Treatment of posterior segment inflammation (including optic neuritis) involves systemic steroid treatment with a slow taper (i.e., treatment of a 60kg patient for optic neuritis may begin with 60mg prednisone PO for two weeks, then 40mg for two weeks, then decrease by 10mg for two weeks, then keep at 5mg or 2.5mg for two or four weeks, respectively). Taper is dependent on response to treatment and should be comanaged with the oncologist. If there is no improvement in ocular conditions, the drug should be discontinued. Before attributing the ocular condition to drug toxicity, other inflammatory/infectious etiologies should be ruled out with bloodwork, such as ESR, CRP, HSV1/2 titer, RF, QuantiFERON-TB, RPR, ANCA and Lyme, if applicable. Any case of orbital or optic nerve involvement should also have MRI imaging of the brain/orbits.
Patients who develop blurred vision, pain or redness should be seen promptly, including dilated fundus examination. Special attention to the anterior chamber and vitreous will help detect subtle inflammation. Clinically or visually significant findings, including ocular toxicity grading, must be reported to the oncologist as they may impact dosing and treatment, and comanagement with ophthalmology may be needed.
Mitogen-Activated Protein Kinase (MEK) Inhibitors
MEK inhibitors work by blocking the MAPK pathway, which is often dysregulated in human cancers. These drugs are used to treat BRAF v600E mutant melanoma, histiocytic neoplasms and neurofibromatosis type 1, and many MEK inhibitors are now used in combination with BRAF inhibitors for the treatment of certain cancers, increasing the probability of ocular toxicity. Examples of FDA-approved MEK inhibitors include Mekinist (trametinib), Cotellic (cobimetinib), Koselugo (selumetinib) and Mektovi (binimetinib).
Toxicity. MEK inhibitor-associated retinopathy (MEKAR) may occur within the first week of the first dose of MEK inhibitor therapy. This entity is characterized by bilateral, yellow-grey elevations of the retina, circular in configuration without inferior tracking.17 OCT reveals fluid between the interdigitation zone and retinal pigment epithelium in varying configurations (Figure 4). Forty-eight percent of patients with MEKAR will complain of blurred vision and/or metamorphopsia or see a “bubble” in their vision.17 Another potential ocular complication is retinal vein occlusion with an incidence of 0.2%, and predisposing risk factors include glaucoma, uncontrolled hypertension and diabetes mellitus.14
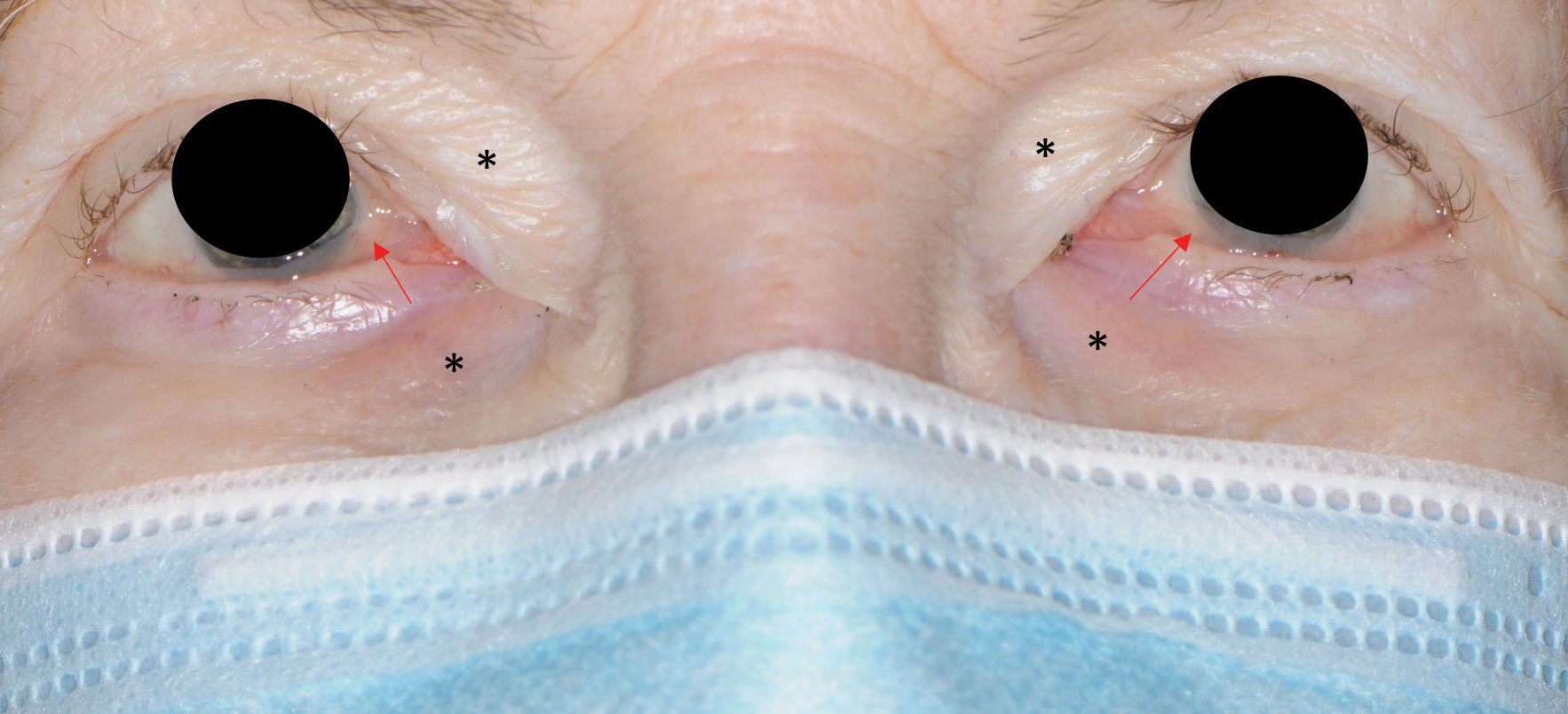 |
Fig. 5. Periorbital edema (black asterisks) and conjunctival chalasis (red arrows) in a patient on Gleevec. Click image to enlarge. |
Treatment and management. In patients who present with MEKAR, it is our clinical experience that the fluid tends to resolve on its own without the need for intervention. However, the drug label instructions should be followed for ocular toxicity: withhold Mekinist and Cotellic in a patient with MEKAR, but the patient may resume the drug if fluid resolves within three to four weeks.17 Patients taking Mektovi only need to pause the drug if they develop MEKAR and experience visual symptoms. In those patients who develop retinal vein occlusion, treatment may involve intravitreal anti-VEGF injection, and they will need to discontinue the drug.
Patients should be monitored regularly and be seen immediately if there is a change in vision. As with other types of agents, it is critical that clinically or visually significant findings, including ocular toxicity grading, must be reported to the oncologist as they may impact dosing and treatment, and comanagement with ophthalmology may be needed.
Selective Estrogen Receptor Modulators (SERMs)
This class of drugs blocks estrogen action by binding to estrogen receptors (ER), thereby treating cancers such as ER+ breast cancer or metastatic breast cancer. Nolvadex or Soltamox (tamoxifen) and Fareston (toremifene) are examples of current FDA-approved SERMs.
Toxicity. Asymptomatic corneal deposits may occur in these patients, although the incidence is less than 0.7%.18 This drug class may also cause irreversible refractile retinal deposits, more commonly as total cumulative doses reach 100g.14 These retinal deposits may cause macular edema and affect vision.
Treatment and management. If corneal deposits are found, continuation of the drug is likely the safest option. However, there is no proven treatment for macular edema associated with tamoxifen, besides discontinuation of the drug. These patients should be monitored regularly and immediately if the patient experiences changes in vision. Clinically or visually significant findings, including ocular toxicity grading, must be reported to the oncologist as they may impact dosing and treatment.
Tyrosine Kinase Inhibitors (TKIs)
Tyrosine kinases phosphorylate amino acids on substrate enzymes, which go on to alter signal transduction pathways. Dysregulation of these pathways is found in many human cancers, and TKIs work by blocking these signals. While there are many TKIs currently on the market, the one most likely to cause ocular toxicity is Gleevec (imatinib). This agent is used to treat leukemia, myelodysplastic disease, hypereosinophilic syndrome, dermatofibrosarcoma protuberans and gastrointestinal stromal tumors.
Toxicity. Mild to moderate periorbital edema occurs in 47% of patients on Gleevec, in addition to conjunctivochalasis as seen in Figure 5.14 This causes poor lid apposition, leading to epiphora. These patients also may experience spontaneous subconjunctival hemorrhages and, in rare cases, retinal hemorrhages, cystoid macular edema and optic nerve edema.
 |
| Click table to enlarge. |
Treatment and management. Treatment of periorbital edema includes topical corticosteroid drops and, in some cases, oral diuretics.19 Epiphora will improve with cessation of therapy. There is no known treatment for optic neuritis in these patients, and the drug will likely need to be discontinued. Patients should be monitored regularly and at the onset of visual symptoms. Clinically or visually significant findings, including ocular toxicity grading, must be reported to the oncologist, and comanagement with ophthalmology may be needed.
Summary
Our patients are on a variety of medications that we have been trained to learn about due to their potential impact on the eye. But as medicine changes, so too should optometry, as we are often the gatekeepers of the visual system.
Here are some helpful tips to ensure you are providing complete care for your patients:
1. Ask for a complete medical history, and if this includes a history of cancer, you should ask the name of the medication(s) the patient might be taking.
2. Google is your friend. It can be hard to remember the names and mechanisms of every new drug. Look up the drug name and class. For example, “Elahere drug class” search results will remind you that this is an antibody drug conjugate and therefore the place you need to check for ocular toxicity is the cornea.
3. If you forget to ask these questions upfront and see something new in the eye—for example, retinal vein occlusion, subretinal fluid, inflammation, etc.—be sure to ask about medications as you formulate your list of differentials because this may help you hone in on a cause for an ocular disorder.
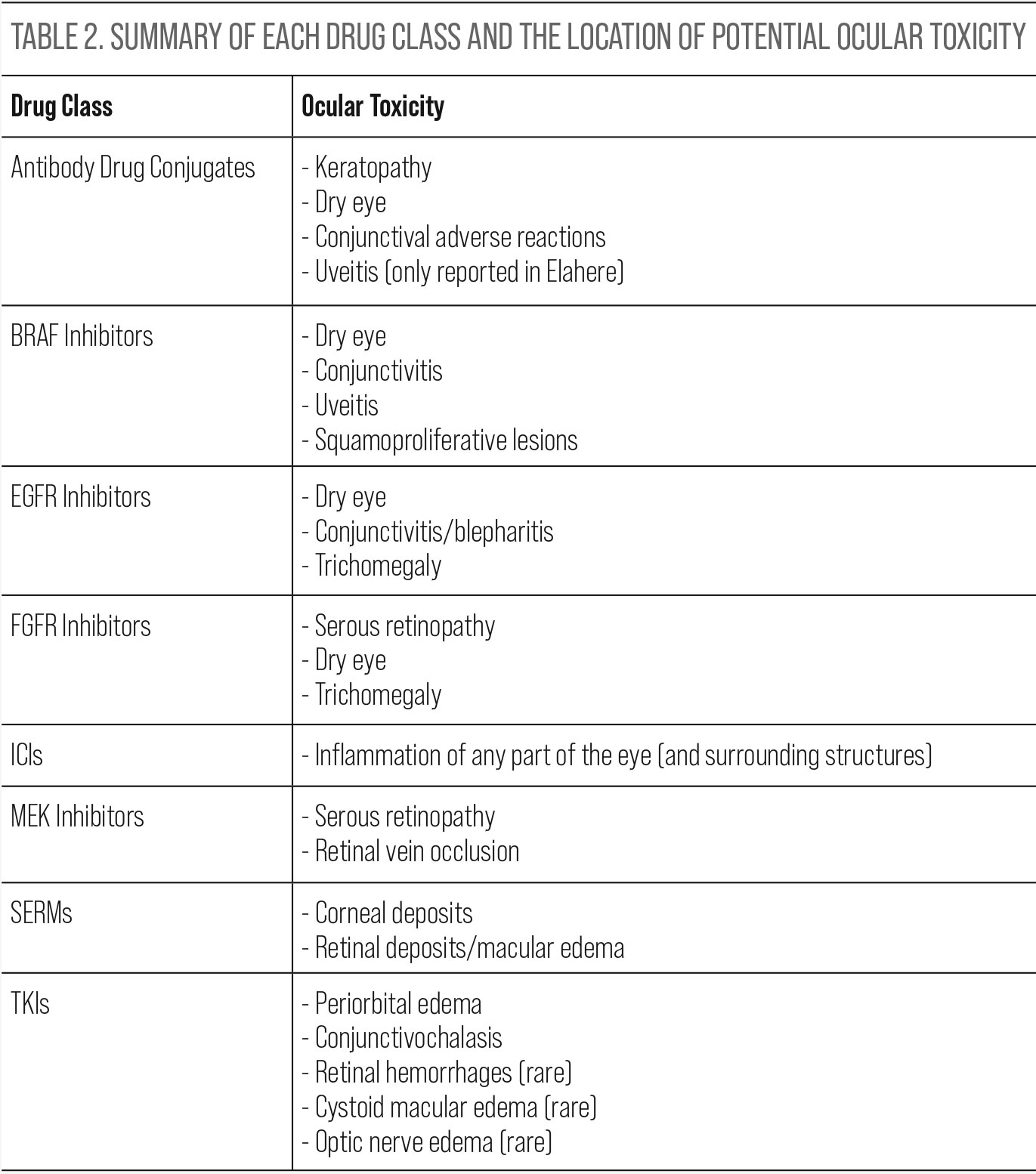
4. Table 2 is a good reference to help remember which parts of the eye may be affected in each drug class.
Dr. Canestraro is an assistant attending optometrist at Memorial Sloan Kettering Cancer Center, Ophthalmic Oncology Service. She has experience in the diagnosis and non-surgical management of ocular disease, including ocular tumors. She also specializes in treating the ocular consequences of cancer and its treatments. She has no relevant financial interests to disclose.
1. Centers for Disease Control and Prevention. US Cancer Statistics: Highlights from 2019 Incidence. 2022. https://www.cdc.gov/cancer/uscs/about/data-briefs/no29-USCS-highlights-2019-incidence.htm. 2. US National Cancer Institute. Common Terminology Criteria for Adverse Events (CTAE) v5.0: keratitis; 2017. 3. Canestraro J, Hultcrantz M, Modi S, et al. Refractive Shifts and Changes in Corneal Curvature Associated With Antibody-Drug Conjugates. Cornea. 2022;41(6):792-801. 4. Kim S, Ursell P, Coleman R, et al. Mitigation and management strategies for ocular events associated with tisotumab vedotin. Gynecol Oncol. 2022;165(2):385-92. 5. Elahere [Package insert]. ImmunoGen Inc, 2022. 6. TIVDAK [Prescribing Information]. Bothell, WA; Seagen Inc. January 2022. 7. Farooq AV, Esposti SD, Popat R, et al. Corneal epithelial findings in patients with multiple myeloma treated with antibody-drug conjugate belantamab mafodotin in the pivotal, randomized DREAMM-2 Study. Ophthalmol Ther. 2020;9(4):889-911. 8. Proietti I, Skroza N, Michelini S, et al. BRAF Inhibitors: Molecular Targeting and Immunomodulatory Actions. Cancers (Basel). 2020;12(7):1823. 9. Choe CH, McArthur GA, Caro I et al. Ocular toxicity in BRAF mutant cutaneous melanoma patients treated with vemurafenib. Am J Ophthalmol. 2014;158(4):831-7.e2. 10. Guedj M, Quéant A, Funck-Brentano E, et al. Uveitis in patients with late-stage cutaneous melanoma treated with vemurafenib. JAMA Ophthalmol. 2014;132(12):1421-5. 11. Belum VR, Rosen AC, Jaimes N, et al. Clinico‐morphological features of BRAF inhibition–induced proliferative skin lesions in cancer patients. Cancer. 2015;121(1):60-8. 12. Singh D, Attri BK, Gill RK, et al. Review on EGFR Inhibitors: Critical Updates. Mini Rev Med Chem. 2016;16(14):1134-66. 13. Borkar DS, Lacouture ME, Basti S. Spectrum of ocular toxicities from epidermal growth factor receptor inhibitors and their intermediate-term follow-up: a five-year review. Support Care Cancer. 2013;21(4):1167-74. 14. Catherine Y Liu, Jasmine H Francis, David H Abramson. Ocular Side Effects of Systemically Administered Chemotherapy. UpToDate. 2022. https://www.uptodate.com/contents/ocular-side-effects-of-systemically-administered-chemotherapy. 15. Francis JH, Harding JJ, Schram AM, et al. Clinical and Morphologic Characteristics of Fibroblast Growth Factor Receptor Inhibitor–Associated Retinopathy. JAMA Ophthalmol. 2021;139(10):1126-30. 16. Canestraro J, Do A, Potash SD, et al. Immune checkpoint inhibitor associated ocular hypertension (from presumed trabeculitis). Am J Ophthalmol Case Rep. 2021;23:101125. 17. Francis JH, Habib LA, Abramson DH, et al. Clinical and Morphologic Characteristics of MEK Inhibitor-Associated Retinopathy: Differences from Central Serous Chorioretinopathy. Ophthalmology. 2017;124(12):1788-98. 18. Pyrhönen S, Ellmén J, Vuorinen J, et al. Meta-analysis of trials comparing toremifene with tamoxifen and factors predicting outcome of antiestrogen therapy in postmenopausal women with breast cancer. Breast Cancer Res Treat. 1999;56(2):133-43. 19. Esmaeli, B., Diba, R., Ahmadi, M, et al. Periorbital Oedema and epiphora as ocular side effects of imatinib Mesylate (Gleevec). Eye. 2004;18:760-2. |
