Fitting Multifocal Contact Lenses for Myopia Control
Release Date:
February 2017
Expiration Date:
February 1, 2020
Goal Statement:
Myopia is the single most significant cause of distance vision impairment, and high myopia (worse than -5.00D) is associated with a number of sight-threatening complications—highlighting the need for strategies and solutions to reduce the risk of onset and slow progression. This article discusses the use of soft contact lenses for myopia control and how to incorporate them into your practice.
Faculty/Editorial Board:
Padmaja Sankaridurg, PhD, BOptom, MIP
Credit Statement:
This course is COPE approved for 1 hour of continuing education credit. Course ID is 52287-CL. Check with your state licensing board to see if this counts toward your CE requirements for relicensure.
Joint-Sponsorship Statement:
This continuing education course is joint-sponsored by the Pennsylvania College of Optometry.
Disclosure Statement:
The author's employer has a commercial interest in myopia control.
Myopia affected approximately one and a half billion people in 2010, and that number is expected to rise to nearly five billion by 2050.1 It is the single most significant cause of distance vision impairment, and high myopia (i.e., worse than -5.00D) is associated with a number of sight-threatening complications such as myopic macular degeneration, retinal detachment, cataract and glaucoma.2-4 This significant burden highlights the need for strategies and solutions to reduce the risk of onset and slow the progression in those already affected by myopia.
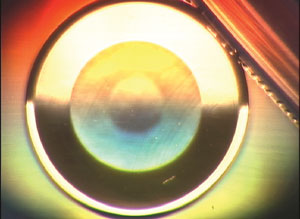 |
| The Proclear center-distance multifocal using the Brien Holden Vision Institute's contact lens optical quality analyzer demonstrates two distinct zones in the optical zone of the lens and a flat peripheral carrier. |
Strategies for Control
Myopia is a complex trait influenced by a number of environmental and genetic factors, and the mechanisms underlying onset and progression are not fully understood. Although there is a great deal to learn about the mechanisms of myopia and why individuals respond differently to different stimuli and treatments, some behavioral, pharmaceutical and optical strategies already show promise in clinical trials in combating myopia—many of which can be incorporated into current day practice.5-26
Prevention is obviously the most effective strategy to reduce the burden of myopia. Several randomized clinical trials suggest a lifestyle intervention with more time spent outdoors reducing the risk of onset.5,6 However, because this involves education and behavioral modification in the years prior to the onset of myopia, comprehensive community-based programs that involve parents, caregivers, teachers, governmental and non-governmental organizations and eye care practitioners (ECPs) must be implemented for this approach to be effective. Despite the crucial role ECPs play in educating parents and communities, their role is limited by the fact that first contact with a practitioner usually comes after the onset of symptoms and signs.
Once a patient is diagnosed with myopia, the ECP becomes the central care provider and is integral to evaluating the risk of further progression. ECPs now have many options for correcting distance vision impairment and slowing its progression. These options include more time spent outdoors, atropine therapy (including low-dose atropine 0.01%), spectacles (progressives, peripheral defocus management and executive bifocals), contact lenses that impose myopic defocus across sections of the retina, and orthokeratology.5-26
Of these various interventions, contact lenses fare well in terms of the risk-benefit ratio compared with other interventions for myopia control. For example, atropine has greater efficacy rates but an increased risk of side effects compared with contact lenses; in addition, myopia rebounds once treatment is stopped.7,8 Clinical trials and case studies show specially designed contact lenses slow myopia progression from 25% to 72% compared with spectacles.9-21
Contact lenses used for myopia control can be either bifocal or multifocal soft contact lenses, as well as the rigid contact lens designs used in orthokeratology. Investigators have proposed several mechanisms to explain their myopia control effect, including: (1) contact lenses correct or reduce accommodative lag, which is considered a stimulus for eye elongation; (2) they reduce the peripheral retinal defocus, which is considered to increase the risk of eye elongation by shifting the image closer to the retina; and (3) the lenses impose myopic defocus across areas of the retina, which is considered to inhibit eye growth.16-21,25,26
These practice pearls can help you better understand the use of soft contact lenses for myopia control and how to incorporate them into your practice. Currently, no products are on the market specifically for use in myopia control; thus, this discussion is based on clinical trial data on the use of multifocal contact lenses for myopia control.
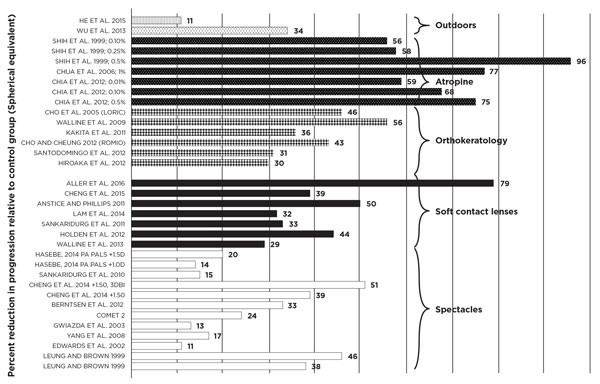 |
| Myopia control with various interventions. Note the efficacy of these interventions compared with standard, single vision spectacles or contact lenses. |
Where to Begin
All individuals presenting with myopia should be assessed for risk of progression based on age, ethnicity, family history of myopia and past history of progression. The ocular examination should include a cycloplegic assessment of the refractive error. A non-cycloplegic refraction often results in a more myopic refraction, and the difference is greatest in younger children and those with low myopic, emmetropic and hyperopic refractive errors.27 Because of this, ECPs should note that a patient without myopia could be classified incorrectly as having myopia; likewise, the magnitude of myopia could be found to be higher than it actually is in a patient with myopia.
ECPs can decide to fit contact lenses based on an assessment of the risk profile or at the request of the patient or, in the case of a child, the caregiver. When fitting contact lenses for myopia control, clinicians should take into consideration the minimum age at which contact lenses can be fitted, contact lens design for myopia control, tests to perform, the wear and care schedule, managing visual performance and follow-up intervals.
Let's take a look at these considerations in more detail:
Fitting Age
Studies show children as young as eight can successfully manage lens insertion, removal and care.17-21,25,28,29 Other clinical studies found children achieved the required duration of lens wear (including full-time lens wear), and the reported duration of lens wear was comparable with that seen in adult contact lens wearers.30 Evidence shows no increased risk of complications associated with lens wear in children compared with adults.30,31 While it is common practice to teach both the child and the parent, the ECP should ensure the child can independently manage all aspects of lens wear before prescribing them.
In addition to correcting and controlling progression of myopia, studies indicate children and teenagers wearing contact lenses had improved quality of life with respect to appearance and satisfaction with correction.29 However, not all children can successfully wear contact lenses. Conditions such as allergic conjunctivitis have an onset in childhood and, in such instances, contact lens wear may aggravate or increase the risk of flare-up. Clinicians should ask about any previous history of allergic or vernal conjunctivitis, and examinations should include an eversion of the tarsal conjunctiva.
Contact Lens Design
Bifocal or multifocal contact lenses have proven effective for myopia control.16-21,25,26
The lens design researchers found effective for myopia control was a center-distance multifocal that had two distinct portions within the optical zone: a central portion that corrected for the distance refractive error and an outer zone that was relatively positively powered compared with the central portion.16-21 The relatively positive power was intended to reduce hyperopic defocus, induce myopic defocus or both across areas of the retina. The tested lenses were experimentally designed with the exception of two trials that used commercially available multifocal soft contact lenses: Acuvue bifocal (center distance, alternating five ring bifocal, Vistakon) and Proclear multifocal D (Coopervision).19,21
Depending on the lens design, the central distance portion varies in diameter, and the relative positive power is delivered as either concentric rings or as a gradient power rising from the center to the periphery. The dioptric magnitude of the relative positive or plus power—which is fixed for use across the population and not individualized—commonly ranging in power from +1.50D to +2.50D. There is still a dearth of information regarding whether increasing the relative positive power or providing individualized treatment is likely to deliver improved myopia control.
Assessing Fit and Performance
The initial lens selection should be based on cycloplegic spherical equivalent refractive error and appropriately adjusted for vertex distance. The contact lenses employed in clinical trials were spherical lenses that masked low amounts of astigmatism (commonly <0.75D and based on the spherical component of the refractive error). Clinicians should refer to the manufacturer's guidelines for lens selection wherever possible.
Patients generally find the first few minutes of lens wear unsettling but tend to adapt quickly. Clinicians should wait to evaluate visual performance until 20 to 30 minutes after lens insertion. To ensure a successful fit, ECPs should examine and optimize the lens centration and movement before addressing visual performance. Issues with lens fit such as decentration or excessive lens movement on the eye may mimic or increase the severity or frequency of symptoms associated with multifocal lens wear such as ghosting, poor contrast and haloes.
Poor visual performance may be related to a number of factors, including: strength of the relative positive power in the optical zone; power profile of the lens (for example, concentric rings of plus power vs. gradient increase in plus power); pupil size; ambient illumination and contrast. A thorough clinical evaluation taking these factors into account may determine if the patient requires a change in lens fit, lens design or simply reassurance that the lens is properly fit. If clinicians perform over-refraction, they should do so using a trial frame rather than a phoropter to minimize errors related to head tilt and movement behind the phoropter.
| Practice Pearls on Myopia Control: |
| 1. Your toolkit for myopia management should include myopia control contact lenses. 2. Assess the risk of progression of myopia for a patient and tailor the management based on the risk. 3. A cycloplegic assessment of the refractive error is essential, particularly in children, as non-cycloplegic refractive assessment often results in a more myopic refractive error. 4. Children eight years and older can successfully be fit with contact lenses and can independently manage and care for their lenses. In children, clinicians should examine the anterior segment before prescribing contact lenses, including eversion and examination of the tarsal conjunctiva. 5. Contact lens designs employed for myopia control are multifocal or multifocal-like lenses with a portion of the optical zone devoted to correcting the distance myopic refractive error and the remainder being relatively positive compared with the distance power by an average of +1.50D to +2.50D. 6. Wait 20 to 30 minutes to allow lenses to settle prior to examining lens fit and visual performance. Optimize lens fit prior to measuring visual performance with the lenses. 7. A daily disposable option or a frequent replacement schedule minimizes the risk of complications associated with contact lens wear. 8. When fitting children with contact lenses, ensure the children can independently manage lens insertion and removal, as well as lens care procedures. |
Wear Time and Replacement Modality
Patients should be advised to wear myopia control contact lenses for all waking hours, as improved lens wear compliance results in better outcomes.18 Also, patients should have an up-to-date spectacle prescription for occasions when lens wear may not be feasible.
Contact lens wear does not appear to pose an increased risk of complications in children compared with adults.32,33 To reduce the risk of complications associated with lens wear, whatever they may be, ECPs should prescribe a regimen that minimizes lens handling and the consequent risk of microbial contamination of the lenses. Education is key, and ECPs should emphasize the risks associated with overnight lens wear such as increased risk of infection and focus on properly training patients in appropriate lens care and handling techniques. A daily wear, daily disposable or frequent replacement schedule is often the most successful approach.
Also, while it is common practice to teach both the child and the parent, practitioners should ensure the child is fully adept at managing all aspects of lens wear such as insertion and removal, lens disinfection as well as taking necessary steps to prevent adverse events, such as avoiding lens wear when unwell or avoiding use of solutions other than those provided by the ECP.
For patients with myopia progression, a three- to six-month follow-up schedule is ideal for avoiding potential adverse effects such as blurred vision. Any drop in visual acuity of one line or more or over-refraction of 0.25D or more necessitates the need for a refractive error assessment so the lens power can be appropriately adjusted.
Our Responsibility
The rising prevalence of myopia and its notably progressive nature is an increasingly significant concern for ECPs and their patients. While further research regarding the underlying mechanisms of myopia is needed, current data points to contact lenses as a safe and effective means of delivering myopia control.9-21 Since progression of myopia is rapid in childhood, treatment strategies should be directed mostly to children and young adults, for whom studies show contact lenses provide a better risk-benefit than other forms of myopia control. Taking into consideration patient expectations and their ability to manage lens wear, ECPs should opt for myopia control contact lenses in treating individuals at risk of onset and progression.
Prof. Sankaridurg is the program leader for the Myopia Program at the Brien Holden Vision Institute. She was awarded her BOpt degree from the Elite School of Optometry, Chennai, India, in 1989, her PhD in 1999 from the University of New South Wales, Australia, and her MIP in 2012 from University of Technology, Australia. After working for a number of years at the L.V. Prasad Eye Institute, India, as the chief of Contact Lens Services, she took a position at the Brien Holden Vision Institute and the Vision Cooperative Research Centre. She was appointed a conjoint professor at the School of Optometry and Vision Science, University of New South Wales, Australia, in 2016. She has been actively researching myopia for approximately 13 years. She is also involved in postgraduate supervision and manages the institute's Intellectual Property portfolio. She has more than 50 articles in peer reviewed journals, is a co-inventor on nine patents/applications, has authored several book chapters and has delivered many podium presentations including keynote lectures.
1. Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036-42.
2. Chen SJ, Cheng CY, Li AF, et al. Prevalence and associated risk factors of myopic maculopathy in elderly Chinese: the Shihpai eye study. Invest Ophthalmol Vis Sci. 2012;53(8):4868-73.
3. Sun J, Zhou J, Zhao P, et al. High prevalence of myopia and high myopia in 5060 Chinese university students in Shanghai. Invest Ophthalmol Vis Sci. 2012;53(12):7504-9.
4. Li T, Du L, Du L. Prevalence and Causes of Visual Impairment and Blindness in Shanxi Province, China. Ophthalmic Epidemiol. 2015;22(4):239-45.
5. Wu PC, Tsai CL, Wu HL, et al. Outdoor activity during class recess reduces myopia onset and progression in school children. Ophthalmology. 2013;120(5):1080-5.
6. He M, Huang W, Zheng Y, et al. Refractive error and visual impairment in school children in rural southern China. Ophthalmology. 2007;114(2):374-82.
7. Chia A, Lu Q, Tan D. Atropine for the treatment of childhood myopia: safety and efficacy of 0.5%, 0.1%, and 0.01% doses (Atropine for the Treatment of Myopia 2). Ophthalmology. 2012;119(2):347-54.
8. Shih YF, Chin CH, Chou AC, et al. Effects of different concentrations of atropine on controlling myopia in myopic children. J Ocul Pharmacol Ther. 1999;15(1):85-90.
9. Edwards MH, Li RW, Lam CS, et al. The Hong Kong progressive lens myopia control study: study design and main findings. Invest Ophthalmol Vis Sci. 2002;43(9):2852-8.
10. Gwiazda J, Hyman L, Hussein M, et al. A randomized clinical trial of progressive addition lenses versus single vision lenses on the progression of myopia in children. Invest Ophthalmol Vis Sci. 2003;44(4):1492-500.
11. Sankaridurg P, Donovan L, Varnas, S, et al. Spectacle lenses designed to reduce progression of myopia: 12-month results. Optom Vis Sci. 2010;87(9):631-41.
12. Leung, JT, Brown B. Progression of myopia in Hong Kong Chinese schoolchildren is slowed by wearing progressive lenses. Optom Vis Sci. 1999;76(6):346-54.
13. Yang Z, Lan W, Ge J, et al. The effectiveness of progressive addition lenses on the progression of myopia in Chinese children. Ophthalmic Physiol Opt. 2009;29(1):41-8.
14. Hasebe S, Jun J, Varnas SR. Myopia control with positively aspherized progressive addition lenses: a 2-year, multicenter, randomized, controlled trial. Invest Ophthalmol Vis Sci. 2014;55(11):7177-88.
15. Berntsen DA, Sinnott LT, Mutti DO, Zadnik K. A randomized trial using progressive addition lenses to evaluate theories of myopia progression in children with a high lag of accommodation. Invest Ophthalmol Vis Sci. 2012;53(2):640-9.
16. Anstice NS, Phillips JR. Effect of dual-focus soft contact lens wear on axial myopia progression in children. Ophthalmology. 2011;118(6):1152-61.
17. Sankaridurg P, Holden B, Smith E 3rd, et al. Decrease in rate of myopia progression with a contact lens designed to reduce relative peripheral hyperopia: one-year results. Invest Ophthalmol Vis Sci. 2011;52(13):9362-7.
18. Lam, CS, Tang WC, Tse DY, et al. Defocus Incorporated Soft Contact (DISC) lens slows myopia progression in Hong Kong Chinese schoolchildren: a 2-year randomised clinical trial. Br J Ophthalmol. 2014;98(1):40-5.
19. Aller TA, Wildsoet C, Results of a one-year prospective clinical trial (CONTROL) of the use of bifocal soft contact lenses to control myopia progression. Ophthalmic Physiol Opt. 2006;26 Suppl 1:1-67.
20. Holden BA, Sankaridurg P, Lazon de la Jara P, et al. Decreasing peripheral hyperopia with distance centre relatively plus powered periphery contact lenses reduced the rate of progress of myopia : A 5 year Vision CRC study. ARVO E abstract 6300. 2012.
21. Walline JJ, Greiner KL, McVey ME, Jones-Jordan LA. Multifocal contact lens myopia control. Optom Vis Sci. 2013; 90(11):1207-14.
22. Hiraoka T, Kakita T, Okamoto F, et al. Long-term effect of overnight orthokeratology on axial length elongation in childhood myopia: a 5-year follow-up study. Invest Ophthalmol Vis Sci. 2012;53(7):3913-9.
23. Cho P, Cheung SW. Retardation of myopia in prthokeratology (ROMIO) study: a 2-year randomized clinical trial. Invest Ophthalmol Vis Sci. 2012;53(11):7077-85.
24. Santodomingo-Rubido J, Villa-Collar C, Gilmartin B, Gutiérrez-Ortega R. Myopia control with orthokeratology contact lenses in Spain: refractive and biometric changes. Invest Ophthalmol Vis Sci. 2012;53(8):5060-5.
25. Aller TA, Wildsoet C. Bifocal soft contact lenses as a possible myopia control treatment: a case report involving identical twins. Clin Exp Optom. 2008;91(4):394-9.
26. Turnbull PR, Munro OJ, Phillips JR. Contact lens methods for clinical myopia control. Optom Vis Sci. 2016;93(9):1120-6.
27. Hu YY, Wu JF, Lu TL, et al. Effect of cycloplegia on the refractive status of children: the Shandong children eye study. PLoS One. 2015;10(2):e0117482.
28. Walline JJ, Jones LA, Rah MJ, et al. Contact lenses in pediatrics (CLIP) study: chair time and ocular health. Optom Vis Sci. 2007;84(9):896-902.
29. Cheng X, Xu J, Chehab K, et al. Soft contact lenses with positive spherical aberration for myopia control. Optom Vis Sci. 2016;93(4):353-66.
30. Walline JJ, Guame A, Jones LA, et al. Benefits of contact lens wear for children and teens. Eye Contact Lens. 2007;33(6.1):317-21.
31. Li L, Moody K, Tan DT, et al. Contact lenses in pediatrics study in Singapore. Eye Contact Lens. 2009;35(4):188-95.
32. Sankaridurg P, Chen X, Naduvilath T, et al. Adverse events during 2 years of daily wear of silicone hydrogels in children. Optom Vis Sci. 2013;90(9):961-9.
33. Chalmers RL, Wagner H, Mitchell GL, et al. Age and other risk factors for corneal infiltrative and inflammatory events in young soft contact lens wearers from the Contact Lens Assessment in Youth (CLAY) study. Invest Ophthalmol Vis Sci. 2011;52(9):6690-6.
