 |
Choroidal Folds: A New Wrinkle in Retinal Care
This often overlooked—yet important—clinical finding can have significant implications for a patient’s overall health.
By Sara Weidmayer, OD
Jointly provided by the Postgraduate Institute for Medicine (PIM) and the Review Education Group
Release Date: June 15, 2023
Expiration Date: June 15, 2026
Estimated Time to Complete Activity: two hours
Target Audience: This activity is intended for optometrists engaged in retinal management of choroidal folds.
Educational Objectives: After completing this activity, participants should be better able to:
Comprehend the anatomy and pathophysiology of choroidal folds.
Recognize choroidal folds via various imaging modalities.
Identify the underlying causes of choroidal folds.
Effectively manage patients who present with choroidal folds.
Disclosure of Conflicts of Interest: PIM requires faculty, planners and others in control of educational content to disclose all their financial relationships with ineligible companies. All identified conflicts of interest are thoroughly vetted and mitigated according to PIM policy. PIM is committed to providing its learners with high-quality, accredited CE activities and related materials that promote improvements or quality in health care and not a specific proprietary business interest of an ineligible company.
Those involved reported the following relevant financial relationships with ineligible entities related to the educational content of this CE activity: Faculty - Dr. Weidmayer has nothing to disclose. Planners and Editorial Staff - PIM has nothing to disclose. The Review Education Group has nothing to disclose.
Accreditation Statement: In support of improving patient care, this activity has been planned and implemented by PIM and the Review Education Group. PIM is jointly accredited by the Accreditation Council for Continuing Medical Education, the Accreditation Council for Pharmacy Education and the American Nurses Credentialing Center to provide CE for the healthcare team. PIM is accredited by COPE to provide CE to optometrists.
Credit Statement: This course is COPE-approved for two hours of CE credit. Activity #126185 and course ID 84777-TD. Check with your local state licensing board to see if this counts toward your CE requirement for relicensure.
Disclosure of Unlabeled Use: This educational activity may contain discussion of published and/or investigational uses of agents that are not indicated by the FDA. The planners of this activity do not recommend the use of any agent outside of the labeled indications. The opinions expressed in the educational activity are those of the faculty and do not necessarily represent the views of the planners. Refer to the official prescribing information for each product for discussion of approved indications, contraindications and warnings.
Disclaimer: Participants have an implied responsibility to use the newly acquired information to enhance patient outcomes and their own professional development. The information presented in this activity is not meant to serve as a guideline for patient management. Any procedures, medications or other courses of diagnosis or treatment discussed or suggested in this activity should not be used by clinicians without evaluation of their patient’s condition(s) and possible contraindications and/or dangers in use, review of any applicable manufacturer’s product information and comparison with recommendations of other authorities.
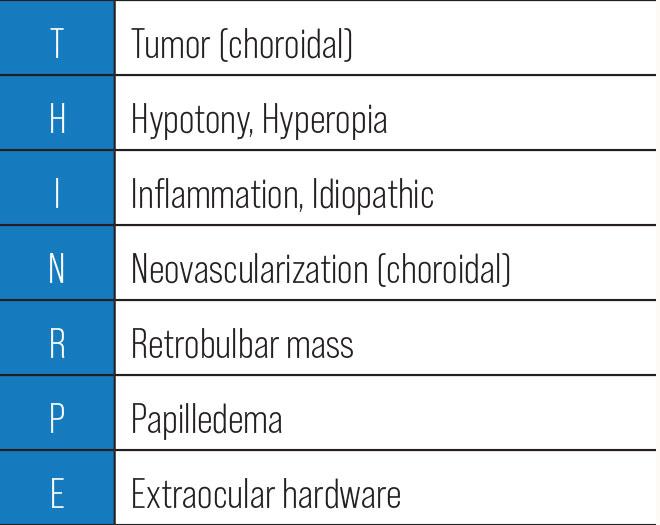 |
| Click table to enlarge. |
While often overlooked as a non-contributory or irrelevant clinical finding, choroidal folds can be associated with serious conditions, both intraocular and extraocular. When we observe choroidal folds clinically, we should never just brush them off but rather ask ourselves what may have caused them to develop in the first place. In most cases, you will find an underlying source if you commit to looking for it.
There’s a simple mnemonic for the basic differentials that may be the source of choroidal folds: THIN-RPE. As we discuss each of these broad categories, remember how important it is to think through the underlying condition causing choroidal folds—this is critical for comprehensive care and positive patient outcomes.
Anatomy & Pathophysiology
Choroidal folds are wave-like crinkles in the inner choroid, overlying Bruch’s membrane (BM), the retinal pigmented epithelium (RPE) and often the outer retina. They present clinically as multiple thin parallel undulations under the retina, whose peaks and troughs make them appear as alternating light/dark bands where the crests are lighter.
When these striations involve the retina as well, they are called chorioretinal folds. Whether choroidal or chorioretinal, our thought process should be the same, so we will refer to them as choroidal folds for the purposes of this article. They are typically seen confined to the posterior pole, most often radiating horizontally from the optic nerve head through the macula; however, they can also be seen at different orientations and in other locations as well.
This clinical finding has patterns that stand out on the imaging modalities optometrists tend to use in-clinic. A classic wavy pattern of the choroid and RPE—and possibly outer retina—is seen on OCT when the line scans are perpendicular to the folds. On OCT angiography (OCT-A), tigroid lines of reduced signal may be seen, presumably due to some stretching and slightly decreased choriocapillaris perfusion along the folds’ trough.1
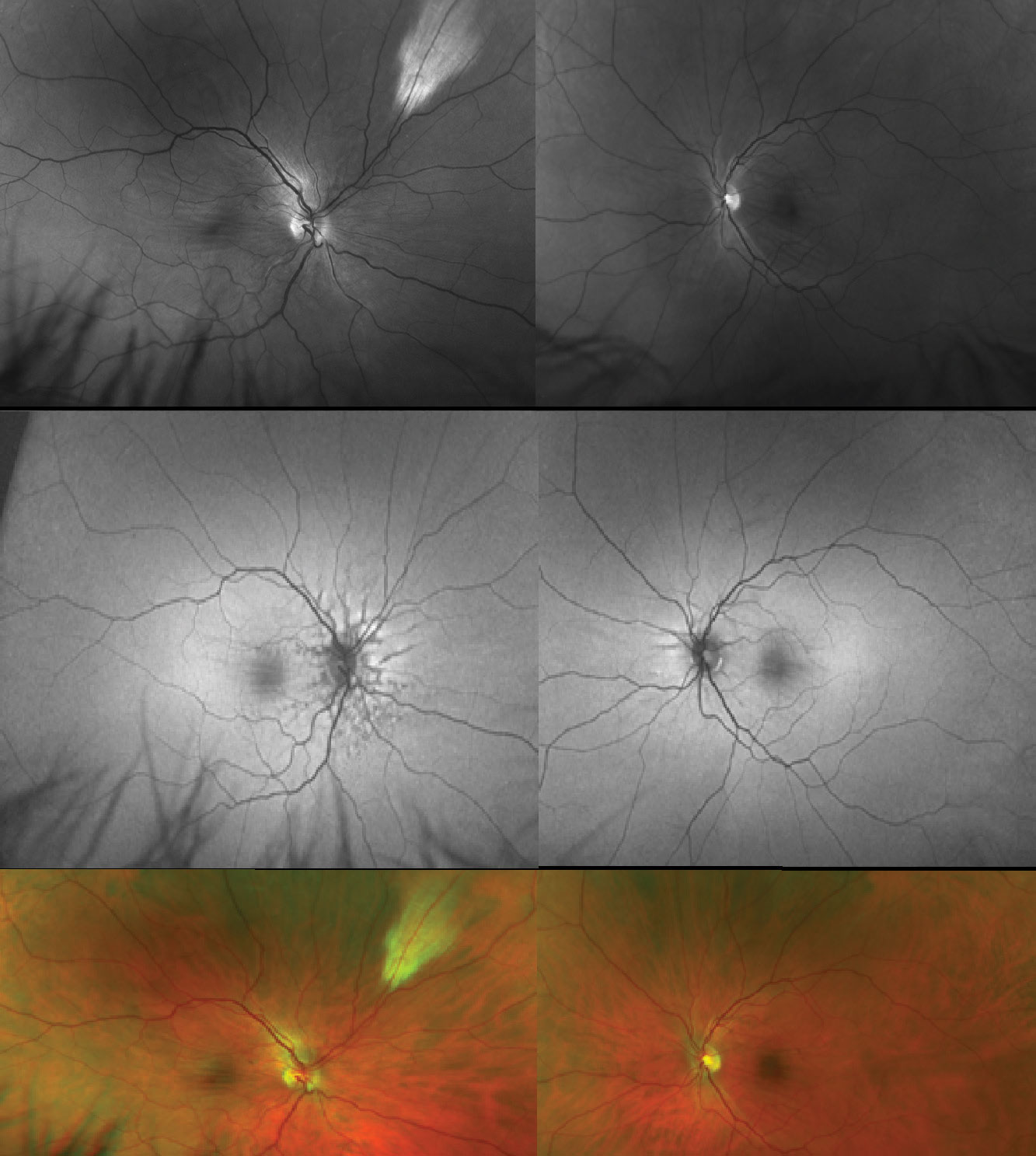 |
Fig. 1. Bilateral choroidal folds radiating from the disc and through the macula with a red-free (green) filter (top), on FAF (middle) and on fundus photos (bottom). Note this patient has angioid streaks around his optic discs OD>OS and myelinated nerve fibers in the superonasal midperiphery OD. Click image to enlarge. |
Fluorescein angiography (FA) shows characteristic background choroidal fluorescence changes due to the RPE and choroidal waves; the troughs appear darker since folded RPE is relatively more dense in the trough, whereas the crests appear more hyperfluorescent because the RPE is slightly stretched and relatively more thin at the apex of the folds. This can be seen as early as the arterial phase or early in the arteriovenous phase on FA.2
On fundus autofluorescence (FAF), we see the opposite hyper-/hypofluorescent pattern as compared with FA. The lipofuscin in RPE cells hyperautofluoresces along the trough where the RPE is relatively more dense and hypoautofluoresces along the crest.
B-scan ultrasonography may not easily detect choroidal folds but can give information about retinal, choroidal and posterior scleral thickness, globe flattening and other relevant information regarding the optic nerve and its sheath, as well as choroidal or retrobulbar lesions that may be contributory. Even without all of these ancillary studies, on our standard fundoscopic exam, choroidal folds stand out when using a red-free (green) filter (Figure 1).
Choroidal folds are typically not associated with visual acuity changes or patient complaints but at times can cause blur or metamorphopsia, especially if the folds develop fairly quickly. However, symptoms may arise from refractive shifts or due to the underlying etiology of the folds.
Broadly, choroidal folds form due to changes in tension on the sclera, choroid, BM or RPE. This change in dynamic leads to the development of folds, largely due to the elasticity and collagenous composition of BM, which allows it to corrugate as it shortens.3 Compressive stress may be due to physical pressure on or around these structures or size changes of these structures. Therefore, when folds are discovered, it is mandatory that they be investigated. The first question should always be, “Why are they there?”
Identifying the Underlying Cause
There are numerous reasons why choroidal folds may form. The mnemonic THIN-RPE can help you remember the broad differentials for the typical causes of choroidal folds, though as you will see, THIN-RPE is not all-inclusive; in fact, it is far from a comprehensive list. We will progress through these etiologies in order of the mnemonic, not in order of frequency, while adding more than the basic THIN-RPE to your list of differentials.
Tumor. Here, we consider choroidal tumors. Choroidal lesions—which take up space, displace the surrounding choroid, compress the sclera from the inside-out and compress the BM-RPE complex from below—can lead to choroidal fold formation.4 Types of choroidal lesions that can lead to formation include cancerous tumors such as melanomas or metastatic lesions, benign tumors or masses such as osteomas or sclerochoroidal calcifications, vascular lesions such as hemangiomas, inflammatory masses such as granulomas and choroidal infiltration from any number of culprits.
While not exactly in the choroid, we must not forget the suprachoroidal space. In this space, suprachoroidal hemorrhages may present. When more localized, they sometimes masquerade as a choroidal mass and can have a similar effect as any choroidal lesion, potentially causing choroidal folds.5 Be especially suspicious of choroidal lesions if the folds do not emanate from the nerve in the typical radial pattern or if there is any adjacent choroidal thickening or color changes.
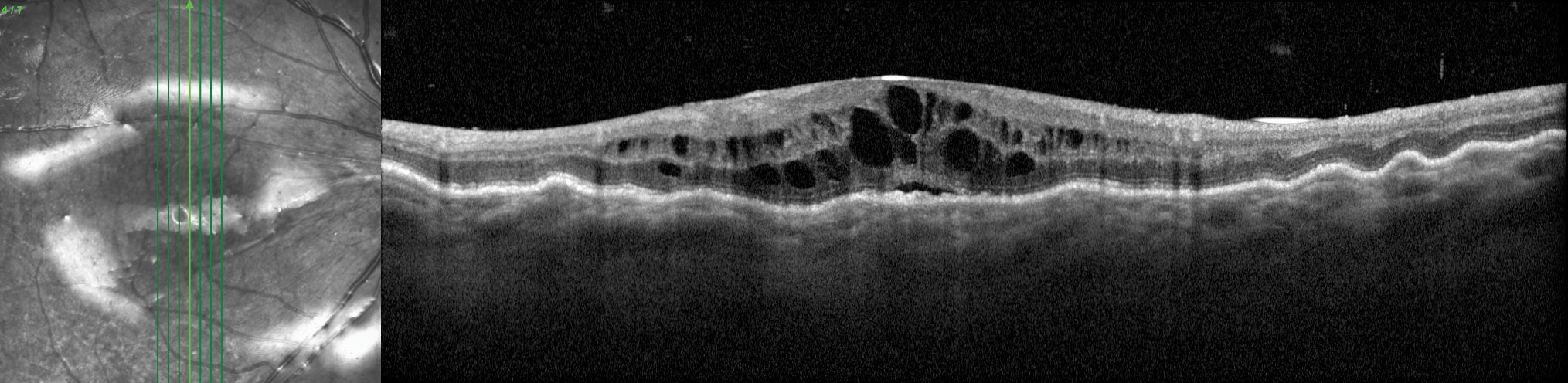 |
Fig. 2. This eye has hypotony maculopathy with choroidal folds, intraretinal and subretinal fluid and optic disc edema. His IOP was generally between 2mm Hg and 5mm Hg. Click image to enlarge. |
Hypotony or Hyperopia. Adequate intraocular pressure (IOP) is critical for maintaining the globe shape. When IOP is very low, there is insufficient counterforce inside the eye to balance the scleral compressive force, so the scleral wall bows or collapses inward. This leads to raisining of the chorioretinal tissue, which is particularly vulnerable in the macula where the thicker parafovea radially folds around the very thin fovea causing hypotony maculopathy (Figure 2).2,6
IOP of about 5mm Hg or less is typically considered hypotony; however, choroidal folds can still occur at pressures that are not quite hypotonous. It is important to note they can occur right before, or along with, the development of other significant side effects of hypotony, such as maculopathy, choroidal effusion or optic disc edema. Thus, choroidal folds seen with low IOP cannot be ignored.
In circumstances of low IOP, the choroidal folds are usually radial around the macula but erratically oriented elsewhere.3 Low IOP-related choroidal folds also beg the question of why the eye is hypotonous (or nearly hypotonous). Here, we must consider factors such as cyclodialysis or intraocular volume loss related to trauma (e.g., open globe) or intraocular surgery (e.g., wound leaks or over-filtration).4
Conditions where choroidal volume is increased or compacted can also lead to choroidal folds. This concept will be touched on in multiple sections, but here we consider hyperopia. Primary hyperopes tend to have shorter axial lengths. This can be conceptualized as the intraocular contents being jammed into an overall smaller package. Choroidal congestion, likely in combination with some redundancy to BM, may cause choroidal folds.7 Intuitively, this is often observed in nanophthalmos.8 Secondary, or induced, hyperopia may also be associated with choroidal folds and will be discussed later.
Inflammation or Idiopathic. It is important to consider inflammatory conditions that affect choroidal thickness, either broadly, such as most forms of choroiditis, uveal effusion or Vogt-Koyanagi-Harada, or more locally, such as in solitary choroiditis. Choroidal folds can also be associated with central serous chorioretinopathy or other points along the pachychoroid spectrum where the choroidal volume is generally greater.
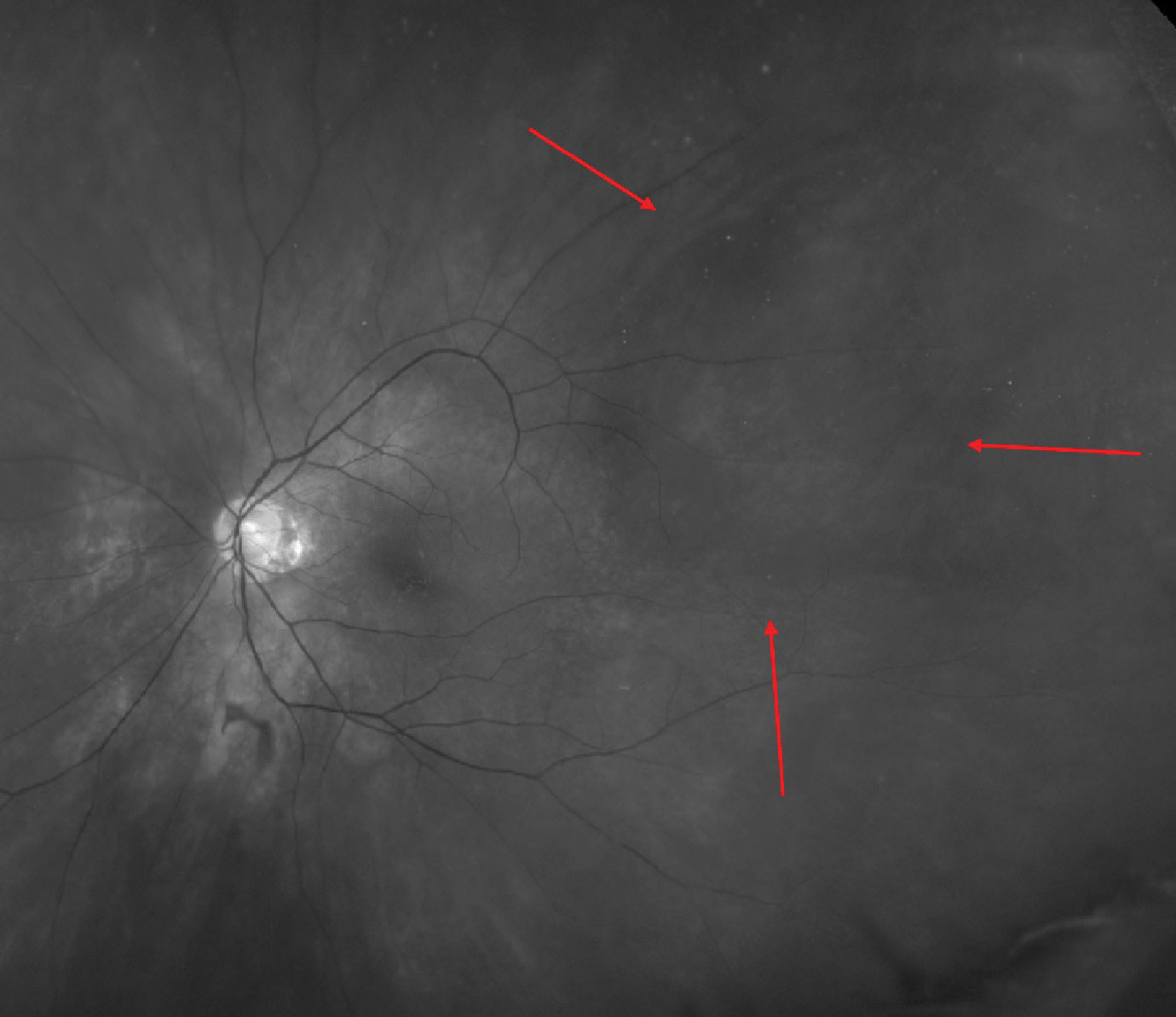 |
Fig. 3. This eye has choroidal folds surrounding a large vortex vein varix, which is more easily visible with a red-free (green) filter. Click image to enlarge. |
Another interesting scenario that could be causative is an increase in the normal pressure within the choroidal vasculature; carotid-cavernous fistulas involve carotid (arterial) blood flow ending up in the cavernous sinus (dural/venous sinus). These can be high or low flow, direct or indirect and may form for a number of different reasons. When higher blood pressure is in the cavernous sinus, this elevates the normal venous pressure in the eye. We most commonly think of increases in the episcleral venous pressure as a result of this and the problems it can cause with IOP, but it could also increase the choroidal vortex venous pressure and vein size, creating a pachychoroid size and pressure effect, which we now know can induce folds (Figure 3).9
Inflammation can also lead to focal or global thickening and later, shrinkage of the sclera itself. One example is posterior scleritis (infectious, inflammatory).4 When actively inflamed, the scleral wall thickens—often along with the choroid—and folds can be induced in this phase; however, as inflammation resolves, the sclera may contract, and folds can evolve as well. Furthermore, they may remain present indefinitely after scleritis resolves.
The overall rigidity of the sclera can also be decreased in some situations, influencing the eye wall’s overall tension and dynamic with the choroid and surrounding structures. We see this especially in younger patients who have long axial lengths—myopes. Myopia isn’t often thought of as a cause of choroidal folds; however, axial myopia and other causes of scleral thinning can also be the offender. Similarly, these folds can also be seen emanating from the edges of posterior staphylomas where the scleral wall is thin and bowed posteriorly.10
It is easy to assume that choroidal folds are idiopathic; however, idiopathic is a diagnosis of exclusion. Chalking choroidal folds up as idiopathic without a workup is bad practice—and a significant liability. Moreover, only about 15% of choroidal fold cases are actually idiopathic.11,12
Even with idiopathic folds, there are some thoughts as to the pathogenesis not being idiopathic at all but rather related to subclinical posterior scleral inflammation in childhood or even in utero. This ultimately causes the sclera to contract and choroidal folds to form.4,13 The patient may also have had a prior—perhaps even insidious—inflammatory condition of the eye or orbit that could have led to scleral thickening or flattening causing folds.4 Regardless, actual idiopathic cases are typically bilateral, confined to the central posterior pole through the macula, and found in visually asymptomatic, hyperopic males.4
Neovascularization. Choroidal neovascularization (CNV) ultimately tends to cause membranes to contract and scar, either spontaneously or after treatment (e.g., intravitreal injections), altering the adjoining anatomy with local choroidal and RPE tightening. Radial choroidal folds from the edges of the CNV can be seen in these cases.13 As we know, CNV may develop due to a host of conditions. If an optometrist observes early folds but no clear evidence of CNV, such as subretinal fluid or hemorrhage, additional testing (e.g., OCT-A or FA) may be warranted since choroidal folds should raise some suspicion for CNV.
 |
Fig. 4. This coronal CT shows a large right frontal sinus mucocele that eroded through the sinus into the orbit and was making contact with the globe. This is an example of an extraconal intraorbital mass that can cause choroidal folds. Click image to enlarge. |
There are other situations where we see outer retina/RPE/BM complex contraction or scarring, which also may be associated with choroidal folds. This has been reported after diode endolaser for a retinal tear, where deep choroidal and scleral thermal injury produced a chorioretinal scar associated with choroidal folds.14 Likewise, choroidal folds are conceivable with other chorioretinal scars, iatrogenic or otherwise.
Similarly, another condition where there are alterations in BM is angioid streaks (Figure 1). Thickened but brittle BM may break, leaving these cracks in the structure. Not only is the local anatomy changed with the angioid streaks, possibly allowing choroidal folds (or CNV) to develop, but as we know, angioid streaks are associated with several metabolic diseases and connective tissue/collagen vascular disorders.15 These conditions themselves may affect the collagenous and elastic structures of the eye (e.g., BM and the sclera).
Conditions such as pseudoxanthoma elasticum, where the composition of BM or the sclera are abnormal, are prone to progressive calcification with loss of elasticity and fragmentation. This may predispose patients to choroidal folding, lacquer cracks and CNV.16 Several of these systemic disorders may alter the collagenous structures of the eye. Examples include osteogenesis imperfecta, Marfan syndrome and others. Taking a pathophysiological approach to choroidal fold formation allows optometrists to expand their differentials, and when we think like doctors should, we will no longer need to memorize a laundry list of etiologies.
Retrobulbar mass. Space-occupying problems in the orbit that compress the globe or optic nerve from behind may also be the culprit behind choroidal folds. These may arise from the extraconal or intraconal space or from the optic nerve itself, such as in the case of optic nerve gliomas. There are a variety of retrobulbar mass types. They may include things like orbital tumors (e.g., cavernous hemangiomas, meningiomas, metastatic lesions), mucoceles originating from the paranasal sinuses or retrobulbar hemorrhages (Figure 4).
Folds from these sources may be seen in non-central locales, though not necessarily at the site of the retrobulbar mass contact, and at unusual orientations, which should raise some flags of suspicion. Other clues may include refractive shifts, more likely hyperopic shifts from intraconal masses pushing the globe relatively more anterior, or astigmatic shifts from extraconal masses abutting the globe. This is most likely to be a unilateral problem—another red flag.
When it comes to retrobulbar masses, we should also consider an increase in pre-existing orbital tissue—processes like thyroid orbitopathy where we may see an increase in extraocular muscle or orbital fat mass, for example.4 Other causes of orbital congestion or edema, such as orbital infections (e.g., orbital cellulitis) or inflammation (e.g., idiopathic orbital inflammation) could also cause choroidal folds to form. The lacrimal gland is another structure stationed around the eye that could enlarge and compress the globe. Any type of dacryoadenitis (infectious, infiltrative, inflammatory, neoplastic) would have to be significant; however, even an enlarged lacrimal gland can press on the globe and deform it enough to cause choroidal folds.17
Papilledema. Things that may cause the optic nerve head to be congested or swollen may lead to compression of the choroid adjacent to the optic disc—another possible culprit of choroidal folds. Any variety of optic disc edema (e.g., ischemic optic neuropathy, papillitis, optic neuritis) can be the inciting factor, including papilledema—bilateral optic disc edema due to intracranial hypertension. Alarmingly, even in the absence of clinically detectable papilledema, choroidal folds can develop due to intracranial hypertension.11,12 It is important to restate that there can be choroidal folds due to intracranial hypertension even though the optic discs may look normal.
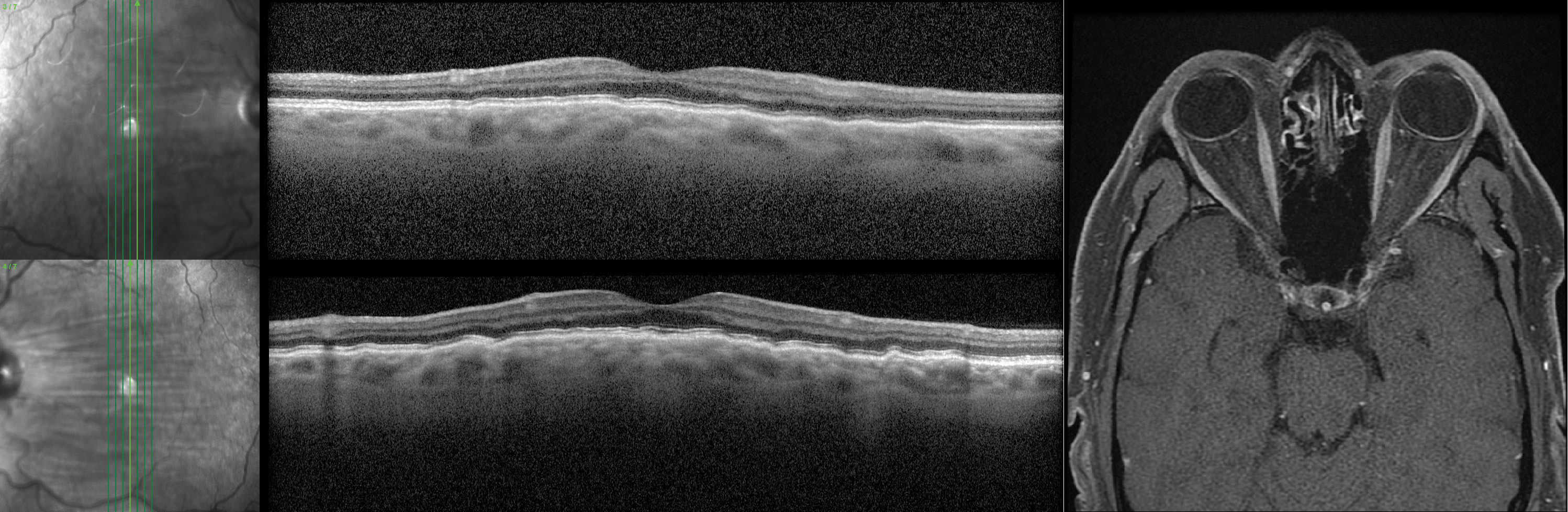 |
Fig. 5. These bilateral choroidal folds OS>OD were found in a male patient in his 40s. He was asymptomatic, moderately hyperopic and had no notable ocular history. His MRI (axial T1) showed posterior globe flattening OD>OS. Click image to enlarge. |
The optic nerve is surrounded by cerebrospinal fluid (CSF) within its sheath, and increased CSF pressure can be induced by things such as dural venous sinus thrombosis, intracranial masses or idiopathic intracranial hypertension among others. Increased CSF pressure changes tautness on the optic nerve and at the optic nerve head, which causes the posterior globe flattening often seen in papilledema.
In some of these cases, we may also see a hyperopic shift. However, even without overt bilateral optic disc edema, increased—or increasing—CSF pressure may begin to have effects on the globe, including choroidal fold formation, even before any axonal swelling or axoplasmic stasis. And, as with other causes of choroidal folds, these folds may stay permanently, even after disc edema or papilledema resolves.
Here, along with choroidal folds radiating from the disc, the choroidal folds are often concentric, like rippling waves from a stone’s throw, around the disc. This orientation of folds may be called Paton’s Lines, though Paton’s Lines can actually be peripapillary retinal folding rather than, or along with, choroidal folds. Optometrists should consider choroidal folds encircling the optic disc as another warning sign.
A brain MRI, magnetic resonance venogram and lumbar puncture may not be necessary to rule out intracranial hypertension in every patient without overt papilledema who has choroidal folds; however, all should be on your radar. In a prospective study, researchers reported that five out of six patients who had choroidal folds without papilledema were found to have intracranial hypertension on lumbar puncture.12 Though only a small study with several limitations, it should still inform management.
In the absence of another clear cause of choroidal folds, patients should be asked about symptoms of intracranial hypertension such as headaches, nausea, vomiting and transient or positional visual obscurations. Baseline structural and functional measurements of the optic nerves should be taken (e.g., OCT and visual fields) with short-interval serial testing to monitor for change. If available, B-scan ultrasonography can also be helpful here, assessing for posterior globe flattening, retrobulbar optic nerve or nerve sheath changes that may be suggestive of increased CSF pressure (Figure 5).
Extraocular hardware. Scleral buckles cinch the globe enough to lessen its circumference. However, narrowing its girth lengthens it in the opposite direction. A scleral buckle stretches the sclera and can cause choroidal folds perpendicular to the buckle’s encirclement.18
Other examples of extraocular hardware may include glaucoma drainage devices or radiotherapy plaques. While not hardware, trabeculectomy also induces changes in the scleral structure and may lead to folds—even if the eye is not over-filtrated and has normal IOP.
One might also consider strabismus surgery. Relocation of typical muscle insertions could also influence the normal scleral tension balance. We may also see choroidal folds after therapeutic scleral windows have been made.
Takeaways
As optometrists, we must remember that choroidal folds are a key clinical finding and shouldn’t be a stand-alone diagnosis—akin to how symptoms are symptoms, not diagnoses, and you must find the reason for them. When we begin to think mechanistically as to why choroidal folds may form, we no longer find ourselves needing to remember lists of possible causes.
A comprehensive knowledge of anatomy and pathophysiology is critical. Even as we use THIN-RPE as a framework for discussing choroidal folds, think outside of the THIN-RPE box about modes of genesis for folds, and internalize the fact that choroidal folds have a plethora of sources beyond the obvious or idiopathic.
Dr. Weidmayer practices at the LTC Charles S. Kettles Medical Center, VA Ann Arbor Healthcare System in Ann Arbor, MI. She is also a clinical assistant professor for the Department of Ophthalmology and Visual Sciences, WK Kellogg Eye Center of the University of Michigan. She has no financial disclosures. The views expressed by the author do not necessarily reflect the position of the US government or Department of Veterans Affairs.
1. Del Turco C, Rabiolo A, Carnevali A, et al. Optical coherence tomography angiography features of chorioretinal folds: a case series. Eur J Ophthalmol. 2017;27:e35-8. 2. Costa VP, Arcieri ES. Hypotony Maculopathy. Acta Ophthalmol Scand. 2007;85(6):586-97. 3. Bullock JD, Egbert PR. Experimental choroidal folds. Am J Ophthalmol. 1974 Oct;78(4):618-23. 4. Agrawal M, Tripathy K. Choroidal Folds. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan. 2022 Aug 22. https://www.ncbi.nlm.nih.gov/books/NBK557772/ 5. Oli A, Balakrishnan D. Multimodal Imaging in a Case of Localized Suprachoroidal Hemorrhage. J Ophthalmic Vis Res. 2020 Jan-Mar;15(1):104-8. 6. Gass JD (1972): Hypotony maculopathy. In: Bellows JG (ed.) Contemporary ophthalmology. Honoring Sir Steward Duke-Elder. Baltimore: Williams & Wilkins 343-66. 7. Kalina RE, Mills RP. Acquired hyperopia with choroidal folds. Ophthalmology. 1980 Jan;87(1):44-50 8. Carricondo PC, Andrade T, Prasov L, Ayres BM, Moroi SE. Nanophthalmos: A Review of the Clinical Spectrum and Genetics. J Ophthalmol. 2018;2018:2735465. 9. Akasaki Y, Inomata T, Sung J, Ito M, et al. Choroidal folds associated with carotid cavernous fistula: a case report. Int J Ophthalmol. 2022;15(11):1881-4. 10. Ishida T. Shinohara K, Tanaka Y, Moriyama M, et al. Chorioretinal folds in eyes with myopic staphyloma. Am J Ophthalmol. 2015 Sep;160(3):608-13.e.1. 11. Musetti D, Nicolò M, Bagnis A, Traverso CE. Chorioretinal folds: associated disorders and a related maculopathy. Am J Ophthalmol. 2014 Aug;158(2):409. 12. Griebel SR, Kosmorsky GS. Choroidal folds associated with increased intracranial pressure. Am J Ophthalmol. 2000 Apr;129(4):513-6. 13. Gass JD. Radial chorioretinal folds. A sign of choroidal neovascularization. Arch Ophthalmol. 1981 Jun;99(6):1016-8. 14. Diskin J, Maguire AM, Margherio RR. Choroidal folds induced with diode endolaser. Arch Ophthalmol. 1992 Jun;110(6):754. 15. Topal T, Düzgün E. Chorioretinal Folds Associated With Different Etiologies. Biomed J Sci & Tech Res. 2018;2(4):2740-6. 16. Roach ES, Islam MP. Pseudoxanthoma elasticum. Handb Clin Neurol. 2015;132:215-21. 17. Kurokawa T, Hamano H, Muraki T, Uehara T, et al. Am J Ophthalmol Case Rep. 2018 Jan 10;9:88-92. 18. Friberg TR. The etiology of choroidal folds. A biomechanical explanation. Graefes Arch Clin Exp Ophthalmol. 1989;227(5):459-64. |
