Antibiotics in Eye Care: A Balancing Act
Here’s what you need to consider when weighing the benefits vs. the risks in the era of resistance.
By Tracy Offerdahl, PharmD, BSc, and Greg Caldwell, OD
 |
Release Date: October 15, 2020
Expiration Date: October 15, 2023
Estimated Time to Complete Activity: 2 hours
Jointly provided by Postgraduate Institute for Medicine (PIM) and Review Education Group
Educational Objectives: After completing this activity, the participant should be better able to:
- Describe the balance necessary to improve the patient’s condition without building antibiotic resistance.
- Appropriately prescribe antibiotics for conditions that warrant them.
- Decide which antibiotic strategy is best for common conditions.
- Discuss contraindications and possible side effects of antibiotics.
Target Audience: This activity is intended for optometrists engaged in the care of patients with corneal dystrophies.
Accreditation Statement: In support of improving patient care, this activity has been planned and implemented by the Postgraduate Institute for Medicine and Review Education Group. Postgraduate Institute for Medicine is jointly accredited by the Accreditation Council for Continuing Medical Education, the Accreditation Council for Pharmacy Education, and the American Nurses Credentialing Center, to provide continuing education for the healthcare team. Postgraduate Institute for Medicine is accredited by COPE to provide continuing education to optometrists.
Faculty/Editorial Board: Tracy Offerdahl, PharmD, BSc, Pennsylvania College of Optometry, and Greg Caldwell, OD, Optometric Education Consultants.
Credit Statement: This course is COPE approved for 2 hours of CE credit. Course ID is 69696-PH. Check with your local state licensing board to see if this counts toward your CE requirement for relicensure.
Disclosure Statements:
Dr. Offerdahl has nothing to disclose.
Dr. Caldwell has received fees from Allergan, Optovue, BioTissue, Envolve, Alcon, Sun Pharma, Eyenovia, Maculogix and Telasight for non-CE/CME services.
Managers and Editorial Staff: The PIM planners and managers have nothing to disclose. The Review Education Group planners, managers and editorial staff have nothing to disclose.
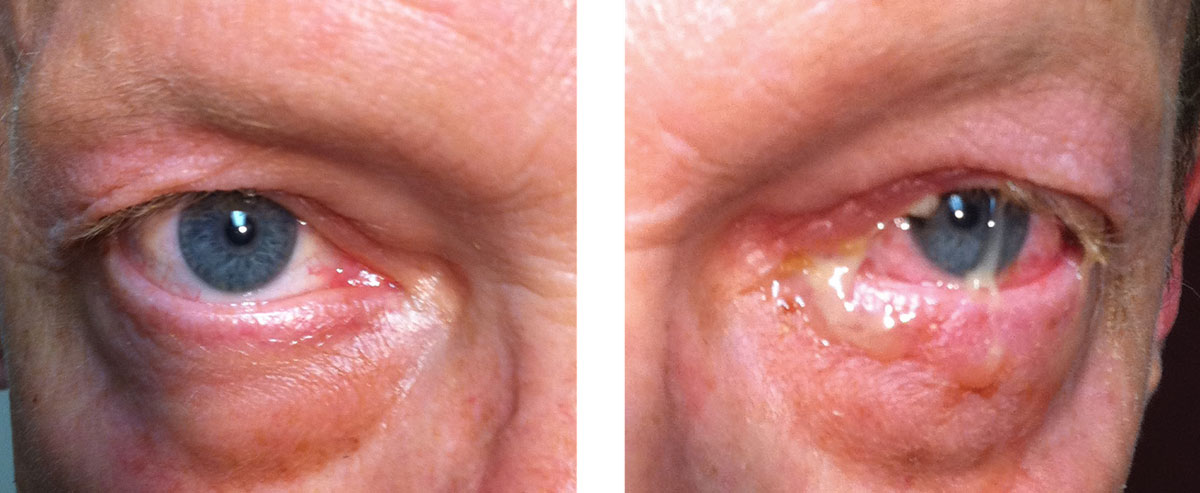 |
| This patient’s examination reveals acute bacterial conjunctivitis. Despite the severity of this infection, the location is limited to the conjunctiva, so using a topical antibiotic is an acceptable treatment choice. Appropriate topical choices include Polytrim, a fluoroquinolone (ciprofloxacin, ofloxacin) or tobramycin.1-4 Click image to enlarge. |
Although antibacterial drugs have been a boon for treating ocular infections, the downside—resistance—always looms in the shadows. Optometric physicians must educate themselves to become cautious and judicious prescribers of these agents.
Antibiotics have long been the cornerstone of treatment to stop infections caused by bacteria, and with many different types of agents, practitioners have a number of choices. The agents categorized as “narrow” tend to treat only one or two bacterial strains, while “broad” agents treat a few to many bacterial strains. We are fortunate to have a category of antibiotics categorized as “multi-drug resistant,” which should be reserved for infections for which we have no typical choices available.
In general, clinicians should use an agent with a spectrum of activity that is wide enough to eliminate the bacteria without being so broad that it destroys the normal flora of the gut biome or sets bacterial resistance in motion. This balancing act requires the clinician to constantly monitor bacterial susceptibilities, resistance patterns, new drug interactions, contraindications and adverse effects.
Another practical consideration includes ensuring that the antibacterial agent is able to reach the site of infection in the eye and surrounding ocular tissues. This is particularly important for the optometrist who often must choose between topical and oral agents when treating bacterial ocular infections.
Table 1. Likely Organisms Responsible For Ocular Infections3,35-38,41 | |
| Conjunctivitis | Staphylococcus aureus Staphylococcus epidermidis Streptococcus pneumoniae Haemophilus influenzae |
| Dacryocystitis | Staphylococcus aureus Staphylococcus epidermidis Streptococcus pneumoniae Pseudomonas aeruginosa |
| Hordeolum | Staphylococcus aureus Staphylococcus epidermidis |
| Preseptal cellulitis | Staphylococcus aureus Staphylococcus epidermidis Streptococcus pneumoniae Haemophilus influenzae |
Oral vs. Topical
Some ocular infections should be treated with an oral antibacterial agent as standard of care, including hordeolum, preseptal cellulitis and dacryocystitis. Oral antibacterial agents provide high systemic levels, which results in better penetration of the agent into the lacrimal apparatus and surrounding tissues.1-3
On the other hand, bacterial infections of the cornea and conjunctiva are adequately treated with a topical agent. Topical application produces higher local concentrations, fewer systemic adverse events, lower risk of resistance and little to no effect on the gut microbiome. Additionally, if it is a non-purulent presentation, a viral pathogen is likely, and an antibacterial agent is not warranted. This simple prescribing strategy is proven to decrease the spread of resistant organisms.3-5
The most common infectious organisms associated with ocular infections are gram-positive isolates, including Staphylococcus aureus, Staphylococcal epidermidis and Streptococcus pneumoniae. Gram-negative organisms may also be present and include Haemophilus influenzae and, less likely, Pseudomonas aeruginosa (Table 1).3,6-8
Patient Considerations
Many patient-specific issues affect the clinician’s medication choices:
Pregnancy/lactation. An important consideration for any prescribing practitioner is the safety of a systemic agent in patients who are pregnant or nursing. In 2015, the Food and Drug Administration (FDA) discontinued the use of the historic pregnancy and lactation letter categories A, B, C, D and X (where A is considered the safest and X is absolutely contraindictated) for all prescription drugs. The main reason for this change is because the historic letter categories are often considered confusing and overly simplistic.9
The new Pregnancy and Lactation Labeling Rule (PLLR), which went into effect on June 30, 2015, provides important information not only for pregnancy and lactation, but also adds a category that evaluates whether or not a prescription drug has any potential reproductive risk in males and females of reproductive age. While many prescription drugs currently have both a letter and PLLR designation, this is temporary, as the FDA has implemented a plan to completely eliminate the letter categories over the next few years.9
 |
| This patient presented with a typical acute bacterial conjunctivitis. Empirically treating for a bacteria rather than a virus would be the optimal choice due to the purulent exudate. A topical antibiotic would be an acceptable treatment option. Appropriate topical choices include polymyxin B + trimethoprim, a fluoroquinolone (ciprofloxacin, ofloxacin) or tobramycin.1-4 If this patient has a penicillin or sulfa allergy, all of these agents would still be appropriate. If the patient is pregnant or breastfeeding, all of these agents would still be appropriate due to little/no systemic absorption. Click image to enlarge. |
Allergies. Medical practitioners in every discipline know that penicillin allergies often emerge when obtaining a patient’s history. However, these allergies aren’t always black and white, and it is sometimes difficult to interpret a patient’s description of their penicillin allergy. The current medical literature is murky on what constitutes a true allergy, and any concrete interpretation of risk and cross reactivity is hard to find. A valuable piece of information comes from the patient’s description of their allergy, so practitioners must always investigate the specific nature of the allergic reaction. It is estimated that 90% of patients who claim to be allergic to a penicillin are not actually allergic.3,10-15
A provider should always approach an allergy with caution and watch for any signs of a Type 1 hypersensitivity reaction. Symptoms of concern include a “wheal-and-flare” rash, swelling of the face, throat or mouth or any respiratory problems such as wheezing or shortness of breath. Patients with any of these issues should avoid drugs in the penicillin class.14,15
Table 2. Dosing Regimens for Community-Acquired MRSA31-34,42 | |
| Sulfamethoxazole + trimethoprim | 800mg/160mg; one tablet BID for 10 days |
| Clindamycin | 300mg to 600mg TID for 10 days |
| Doxycycline | 100mg BID for 10 days |
When evaluating the potential of a cross allergy with the cephalosporins, medications that possess the most similar side chains increase the likelihood of a cross-reaction. For example, cephalexin, a first-generation cephalosporin, is more likely to cross-react with a patient who has a penicillin allergy compared with a drug lacking the side chain (e.g., cefuroxime axetil, which is a second-generation cephalosporin). Clinical experience and some studies support this model, so if a patient does describe what appears to be a potentially dangerous allergic reaction to a penicillin, then it seems to be a safer choice to use a cephalosporin in the second or third generation groups.3,12-16
Methicillin-resistant Staphylococcus aureus (MRSA). We see this organism frequently in both the community and hospitals. While sulfamethoxazole + trimethoprim, clindamycin and doxycycline may not be an optometrist’s typical go-to drugs when treating hordeolum, preseptal cellulitis and dacryocystitis, they are important to consider when managing community-acquired (as opposed to hospital-acquired) MRSA infections.
Vancomycin, a super gram-positive antibiotic, is considered the standard for MRSA infections; however, it is reserved for inpatient use because it must be administered intravenously.
When a patient fails traditional therapy that covers Staphylococcus aureus, or when a patient is known to be colonized with MRSA, it is a good time to consider a potential MRSA infection. Additionally, young patients, those who are incarcerated and athletes are increasingly more likely to have a MRSA infection, as are health care workers, patients who are in assisted living homes or patients with a recent hospitalization. Anyone with a history of previous MRSA infection is also at an increased risk since the bacteria can live under our fingernails and in our nasal cavities for years (Table 2).17-19
 |
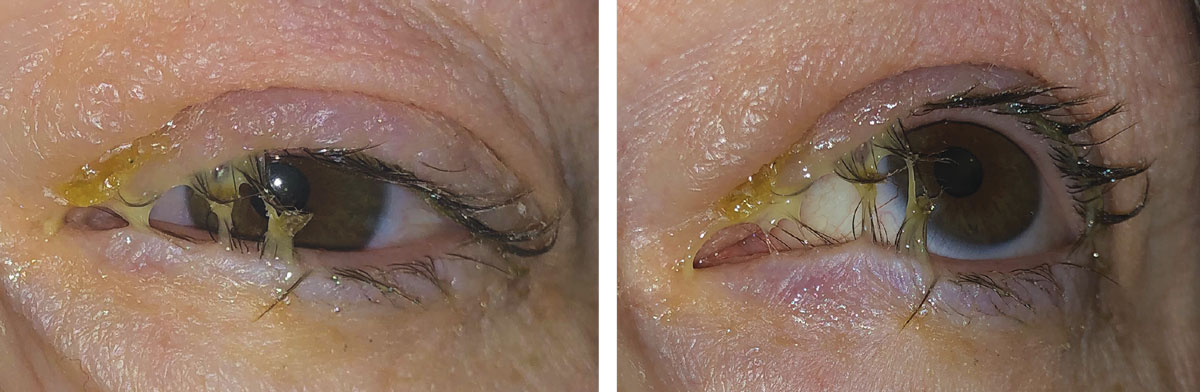
This patient’s examination reveals a hordeolum and preseptal cellulitis. Because the hordeolum is like an abscess and the preseptal cellulitis involves the skin/skin structures, an oral antibiotic is appropriate. Fever or other systemic signs/symptoms of infections may warrant hospitalization with intravenous antibiotics. Appropriate systemic agents include Augmentin, Keflex, azithromycin or Bactrim. When none of these agents can be used due to allergy, a fluoroquinolone (levofloxacin, moxifloxacin) may be considered. If there is concern regarding the potential for MRSA, systemic options include Bactrim, doxycycline or clindamycin.1-4,32-34,42 If this patient has a severe, life-threatening penicillin allergy (Type 1 hypersensitivity), Augmentin would be contraindicated and Keflex should also be avoided.6-9,11-16 If they have a mild reaction to penicillin (mild, non-descript rash), Keflex may still be considered a safe choice.6-9,11-16 Bactrim is contraindicated in patients with a sulfa allergy.32-34 Augmentin, Keflex and azithromycin are safe for pregnant or breastfeeding patients while Bactrim and fluoroquinolones are contraindicated.32-40 |
Antibacterial Resistance
Resistant organisms continue to appear at a rate faster than science and research are able to produce new antibiotics to fight them. The World Health Organization’s Global Action Plan on Antimicrobial Resistance plan emphasizes the importance of education, surveillance and research to combat growing bacterial resistance.20
The main mechanism for bacterial resistance is through genetic mutations and a well-known list of factors that contribute to it, including overprescribing of antimicrobials, agricultural use and prescribing inappropriate or incorrect dosing regimens. Optometric-specific issues of resistance are perpetuated by empirical use of antibacterials, short-course or inadequate dosing of antibacterials and repeated use of the same antibacterial agent in a patient.5,19-24
Augmentin (amoxicillin + clavulanate, GlaxoSmithKline) is a beta-lactam plus beta-lactamase inhibitor combination that is designed to treat one type of resistance in some bacterial isolates. The addition of clavulanate, a beta-lactamase enzyme inhibitor, helps to provide increased protection for the amoxicillin against hydrolysis when it is exposed to infections caused by organisms that produce beta-lactamase. These include Haemophilus influenzae and Moraxella catarrhalis.3,5,10,25
Antibiotic Review
Antibacterials are categorized into four classifications: beta-lactams, protein-synthesis inhibitors, fluoroquinolones and sulfonamides.
The beta-lactams, which include penicillins, combined penicillin/beta-lactamase inhibitors and cephalosporins, are the preferred drug for most ocular conditions due to high efficacy and low toxicity. The mechanism of action is bacterial cell wall synthesis inhibitors.
Protein-synthesis inhibitors—macrolides, tetracyclines, clindamycin and aminoglycosides—bind to either 30S or 50S ribosomal unit on bacteria. Among the macrolides, azithromycin is the drug of choice for most atypical infections.
Table 3. Oral Antibiotic Dosing11,26,27,32,33,35,39-41 | |
| Amoxicillin + clavulanate | 500mg/125mg BID to TID for 10 days 875mg/125mg TID for 10 days* |
| Cephalexin | 500mg BID for 10 days |
| Azithromycin | Two tablets (500mg total) on day one, then 250mg once a day on days two through five |
| Sulfamethoxazole + trimethoprim | Double strength = 800mg sulfamethoxazole and 160mg trimethoprim/tablet One tablet every 12 hours for seven to 10 days |
| Levofloxacin | 500mg daily for 10 days |
| Moxifloxacin | 400mg daily for 10 days |
| Ciprofloxacin | 500mg to 750mg BID for 10 days** |
| *Higher doses of amoxicillin provide better coverage for potential Streptococcus pneumoniae bacteria. This organism is more likely to cause infection in adults with an ocular infection. **Choose only if Pseudomonas aeruginosa is suspected or documented. | |
The mechanisms of action for fluoroquinolones, include bacterial DNA gyrase and topoisomerase inhibitors. Fluoroquinolones have coverage of Pseudomonas.
Sulfonamides, which inhibit sequential steps in folate synthesis, are a good medication choice for skin/soft tissue infections due to MRSA coverage.
It is important to note that no anti-infective provides ideal coverage for all pathogens for all infected sites. Here’s a look at the most common antibiotics used in eye care.
Augmentin.3,10-12 This agent includes a beta-lactam (amoxicillin) combined with a beta-lactamase inhibitor (clavulanate). The addition of the beta-lactamase enzyme inhibitor clavulanate provides increased protection for amoxicillin against Haemophilus influenzae and Moraxella catarrhalis, as well as some anaerobes.10-12 In pus-producing infections, the clavulanate is essential to protecting the beta-lactam ring.
Augmentin is one of our first choices if a systemic agent is needed in an ocular infection since it covers all of the most likely causative organisms. It is safe across all age ranges (beginning at 12 weeks of age) and is generally considered safe for use during pregnancy and lactation (historic category B). This medication is typically well tolerated, with the most common side effects being stomach upset and diarrhea. Taking the medication with food often helps to mitigate these issues. Clinicians should always evaluate a patient’s allergy history prior to use.
Keflex (cephalexin, Advancis Pharmaceutical).10-16,26 This agent is a beta-lactam, first-generation cephalosporin. It is not generally destroyed by beta-lactamase producing organisms. The spectrum of activity against common bacterial organisms is similar to amoxicillin, such as methicillin-sensitive Staphylococcus aureus (MSSA), as well as some gram negatives including Haemophilus influenzae and Moraxella catarrhalis.
It is considered safe for individuals eight weeks of age or older as well as for those who are pregnant or breastfeeding (historic category B). Keflex, which is generally well tolerated, is the drug of choice for blowout orbital fractures at a higher dose of 500mg four times a day.
Clinicians should make sure to evaluate patients’ allergy history prior to prescribing this agent, specifically any allergies that have occurred with a penicillin or other beta-lactam agents. The incidence of allergic cross-reaction between a penicillin and a first-generation cephalosporin ranges from 1% to 10%, with most data and expert opinions leaning on the low end of the estimate.
 |
| This patient has a periorbital skin infection with bacterial purulence. Since the infection involves the skin/skin structures surrounding the eye, an oral antibiotic agent would increase treatment success. Appropriate systemic agents include Augmentin, Keflex, azithromycin or Bactrim. When these agents are contraindicated due to an allergy, a fluoroquinolone (levofloxacin, moxifloxacin) may be considered. If there is concern regarding the potential for MRSA, systemic options include Bactrim, doxycycline or clindamycin.1-4,32-34,42 Click to enlarge. |
Azithromycin.27,28 This agent is a macrolide antibiotic with a decent spectrum of bacterial coverage. It has slightly better coverage for Haemophilus influenzaewhen compared with Augmentin, and its atypical bacterial coverage is better than its gram-positive coverage. Additionally, azithromycin is usually the drug of choice for chlamydial conjunctivitis.29,30 This is another reasonable choice when a systemic agent is needed because it covers all of the likely causative organisms. It’s also a good option for some patients with a presumptive or documented true penicillin allergy.
Systemic azithromycin has a dynamic pharmacokinetic profile. Once it is in the bloodstream, it has a very wide distribution into most tissues and compartments, with the exception of the brain and cerebral spinal fluid. Once distributed, azithromycin tissue concentrations are much higher than they are in simultaneous serum concentrations. Wide distribution coupled with liver and biliary elimination results in an elimination half-life of 40 to 68 hours. This means that when a patient takes the last dose of azithromycin on day five, azithromycin continues to provide high enough tissue concentrations to treat an infection for an additional 1.5 to 2.8 days. In serious infections, however, treatment failure is sometimes an issue.27,28
Safe across all age ranges, this drug can generally be used safely in patients who are pregnant or lactating (historic category B). It is typically well tolerated but can cause stomach upset and diarrhea. Post-marketing surveillance has indicated that azithromycin may cause heart issues, such as prolongation of QT interval and torsades de pointes, which can be fatal. Patients on other drugs that may prolong the QT interval (antipsychotics, antifungals, hydroxychloroquine, etc.) or those with a known arrhythmia are at higher risk.27,28
Bactrim (sulfamethoxazole + trimethoprim, Roche).31-34 This agent is the sulfa antibiotic that some patients may be allergic to. Unlike a penicillin allergy, the sulfa allergic patient should generally be assumed to have significant morbidity and potential mortality associated with exposure to this medication. Additionally, this drug has a decent spectrum of bacterial coverage for Staphylococcus spp. (including community-acquired MRSA), Streptococcus spp. and Haemophilus influenzae.
 |
| A clinical examination reveals acute dacryocystitis. Due to the location of this infection, an oral antibiotic agent is the best option. Appropriate systemic choices include Augmentin, Keflex, azithromycin or Bactrim. In the case of an allergy, a fluoroquinolone (levofloxacin, moxifloxacin) may be considered. When MRSA is a concern, systemic options include Bactrim, doxycycline, or clindamycin.1-4,32-34,42 Click image to enlarge. |
While safe across all ages (beginning at four weeks of age), it should be avoided in patients with a sulfa allergy. Risk of use in pregnant patients cannot be ruled out, as it may cause hyperbilirubinemia in later pregnancy (historic category C). While usually well tolerated, serious allergic reactions may occur, including rash, anaphylaxis, Stevens-Johnson syndrome and toxic epidermal necrolysis.32 Some clinical pearls to remember include:
Bactrim DS (double strength) is more often prescribed for ocular infections compared with single strength.
Sulfamethoxazole and trimethoprim are synergistic when used together, and this increases the bacterial spectrum and the efficacy.
Sulfamethoxazole monotherapy was once widely used as a single agent; however, the development of bacterial resistance has rendered it nearly obsolete. This is seen in a number of treatment failures from some physician groups using topical 10% sulfamethoxazole.
Fluoroquinolones.31,33,35-40 The most widely used agents in this class include moxifloxacin, levofloxacin and ciprofloxacin. The last of these has better (and broad) gram-negative coverage, including Haemophilus influenzae and Pseudomonas aeruginosa but gram-positive coverage is more limited due to resistance. Levofloxacin and moxifloxacin have fair to good gram-positive coverage, including Staphylococcus spp. and Streptococcus spp.
Topical fluoroquinolones are safely used in pregnancy, breastfeeding and in infants and children older than age one. However, oral fluoroquinolones should only be used in patients 18 years or older and are contraindicated in those who are pregnant or breastfeeding due to the risk of arthropathy and cartilage damage (historic category C).
Adverse effects may be severe, and these medications have a black box warning from the FDA. Research shows fluoroquinolones are associated with disabling and potentially irreversible serious adverse reactions that have occurred together, including tendinitis and tendon rupture, peripheral neuropathy and central nervous system effects.35-40
Table 4. Topical Antibiotic Dosing1-4,23-47 | |
| Medication(s) | Dose |
| Polymyxin B + trimethoprim solution | One drop in the affected eye(s) every three hours (maximum of six drops per day) for seven to 10 days. |
| Ofloxacin solution | One to two drops in affected eye(s) every two to four hours for the first 2 days, then one to two drops QID for an additional five days. |
| Ciprofloxacin solution | One to two drops into the affected eye(s) every two hours while awake for two days, then one to two drops every four hours while awake for the next five days. |
| Moxifloxacin solution | One drop in affected eye(s) two to three times a day for seven days. |
| Tobramycin | Mild/moderate infection: One to two drops in the affected eye(s) every four hours for seven to 10 days. Severe infection: Two drops in the affected eye(s) hourly until improvement, then one to two drops every four hours for seven to 10 days. |
Discontinue therapy immediately and avoid the use of fluoroquinolones in patients who experience any of these serious adverse reactions. Because fluoroquinolones have been associated with serious adverse reactions, reserve fluoroquinolones for use in patients who have no alternative.35-40
Miscellaneous topical antimicrobials. Commonly used topical antibiotics include Polytrim (polymyxin B + trimethoprim, Allergan), fluoroquinolones such as ofloxacin, ciprofloxacin or Vigamox (moxifloxacin, Novartis), and tobramycin. While this does not represent a complete list of available agents, it does highlight reasonable choices for the topical treatment of acute bacterial conjunctivitis, since they are applied directly to the infected organ.1-4 These agents are typically considered safe for patients who are pregnant or breastfeeding. In general, adverse effects are minimal and may include eye redness, eye irritation and allergy.
As medical professionals, it is always important to evaluate patients from both a macroscopic and microscopic perspective before making any drug therapy choices. This is more challenging every year as more prescription and over-the-counter medications are approved and marketed to patients in many therapeutic categories. Resistant bacteria add another dynamic to patient care.
Our call-to-arms as antibiotic custodians is to choose an antimicrobial agent only when the chances of a bacterial infection are likely. When we do empirically treat a bacterial infection of the eye, choose an agent that is broad enough to treat the most likely organisms with a treatment duration that will mitigate the infection.
Keeping all of these things in mind will help to ensure that the patient is cured and that few to no resistant bacteria have been let loose in the world. Both of these are important factors for a successful treatment plan.
Dr. Offerdahl is an assistant professor at the Pennsylvania College of Optometry in Elkins Park, PA.
Dr. Caldwell is part owner of Optometric Education Consultants and a practicing optometrist in Pennsylvania.
1. Spear C, Obenchain M. When A Drop Isn’t Enough. Rev Optom. 2015;152(1):38-44. 2. Kabat AG, Sowka JW. Stye vs. Stye. Rev Optom. 2016;153(3):111-3. 3. Offerdahl-McGowan T, Caldwell G. One size won’t fit all: treating ocular infection. Rev Optom. 2018;155(4):52-60. 4. Morrow G, Abbott R. Conjunctivitis. Am Fam Physician. 1998;57(4):735-46. 5. Colgan RC, Powers JH. Appropriate antimicrobial prescribing: approaches that limit antibiotic resistance. Am Fam Physician. 2001;64(6):999-1005. 6. Greenberg RD, Dippold AL. Chapter 31: Eye Emergencies. In: Current Diagnosis and Treatment: Emergency Medicine, 8th ed. Stone KC, Humphries RL, eds. New York, NY: McGraw-Hill; 2017. 7. Vagefi MR. Lids & Lacrimal Apparatus. In: Vaughan & Asbury’s General Ophthalmology, 19th ed. Riordan-Eva P, Augsburger JJ, eds. New York, NY: McGraw-Hill; 2018. 8. Carlisle RT, Digiovanni J. Differential diagnosis of the swollen red eyelid. Am Fam Physician. 2015;92(2):106-12. 9. US Food and Drug Administration. Pregnancy and Lactation (Drugs) Labeling Final Rule. www.fda.gov/drugs/labeling-information-drug-products/pregnancy-and-lactation-labeling-drugs-final-rule. December 3, 2014. Accessed September 25, 2020. 10. Beauduy EC, Winston LG. Beta-lactam & other cell wall- & membrane-active antibiotics. In: Katzung BG, eds. Basic & Clinical Pharmacology, 14th ed. New York, NY: McGraw-Hill; 2018. 11. MacDougall C. Penicillins, cephalosporins, and other β-lactam antibiotics. In: Hilal-Dandan R, Brunton LL, eds. Goodman and Gilman’s Manual of Pharmacology and Therapeutics, 13th ed. New York, NY: McGraw-Hill; 2018. 12. Bhattacharya S. The facts about penicillin allergy: a review. J Adv Pharm Technol Res. 2010;1(1):11-17. 13. Zagursky RJ, Pichichero ME. Cross-reactivity in beta-lactam allergy. J Allergy Clin Immunol Prac. 2018;6(1):72-81.e1. 14. Macy E. Penicillin and beta-lactam allergy: epidemiology and diagnosis. Curr Allergy Asthma Rep. 2014;14(11):476. 15. Prematta T, Shah S, Ishmael FT. Physician approaches to beta-lactam use in patients with penicillin hypersensitivity. Allergy Asthma Proc. 2012;33(2):145-51. 16. Romano A, Gaeta F, Arribas Poves MF, Valluzzi RL. Cross-reactivity among beta-lactams. Curr Allergy Asthma Rep. 2016;16(3):24. 17. Marcinak JF, Frank AL. Treatment of community-acquired methicillin-resistant staph aureus in children. Curr Opin Infect Dis. 2003;16(3):265-9. 18. Quinn R. Rethinking antibiotic research and development: World War II and the penicillin collaborative. Am J Public Health. 2013;103(3):426-34. 19. Barbosa TM, Levy SB. The Impact of antibiotic use on resistance development and persistence. Drug Res Updat. 2000;3(5):303-11. 20. World Health Organization. Global Action Plan on Antimicrobial Resistance. www.who.int/antimicrobial-resistance/global-action-plan/en. Accessed September 25, 2020. 21. Ventola CL. The antibiotic resistance crisis: part 1: causes and threat. PT. 2015;40(4):277-83. 22. Van Boeckel TP, Brower C, Gilbert M, et al. Global trends in antimicrobial use in food animals. Proc Natl Acad Sci USA. 2015;112(18):5649-54. 23. Watkins RR, Bonomo RA. Overview: Global and local impact of antibiotic resistance. Infect Dis Clin North Am. 2016;30(2):313-22. 24. Centers for Disease Control and Prevention. About antimicrobial resistance. www.cdc.gov/drugresistance/about.html. Accessed September 25, 2020. 25. Fuda CC, Fisher JF, Mobashery S. Beta-lactam resistance in Staphylococcus aureus: the adaptive resistance of a plastic genome. Cell Mol Life Sci. 2005;62(22):2617-33. 26. Pragma Pharmaceuticals. Keflex (cephalexin) capsules [prescribing information]. December 2018. 27. Pfizer Labs. Zithromax (azithromycin) 250 mg and 500 mg tablets and oral suspension [prescribing information]. March 2017. 28. MacDougall C. Protein synthesis inhibitors and miscellaneous antibacterial agents. In: Hilal-Dandan R, Brunton LL, eds. Goodman & Gilman’s: The Pharmacological Basis of Therapeutics, 13th ed. New York, NY: McGraw-Hill; 2017. 29. Salopek-Rabatic J. Chlamydial conjunctivitis in contact lens wearers: Successful treatment with single dose azithromycin. Clao J. 2001;27:4:209-11. 30. Katusic D, Petricek I, Mandic Z, et al. Azithromycin vs. doxycycline in the treatment of inclusion conjunctivitis. Am J Ophthalmol. 2003;135:4:447-51. 31. Beauduy C, Winston L. Sulfonamides, trimethoprim, & quinolones. In: Basic & Clinical Pharmacology,14th ed. Katzung B, ed. New York, NY: McGraw-Hill; 2018. 32. Monarch Pharmaceuticals Inc. Septra and Septra DS (sulfamethoxazole and trimethoprim) tablets [prescribing information]. August 2013. 33. Sulfonamides, trimethoprim-sulfamethoxazole, quinolones, and agents for urinary tract infections. In: Hilal-Dandan, Brunton L, eds. Goodman and Gilman’s Manual of Pharmacology and Therapeutics, 2nd ed. New York, NY: McGraw-Hill; 2014. 34. Marcinak JF, Frank AL. Treatment of community-acquired methicillin-resistant staph aureus in children. Curr Opin Infect Dis. 2003;16(3):265-9. 35. Bayer HealthCare Pharmaceuticals Inc; Cipro (ciprofloxacin) [prescribing information]. July 2017. 36. Janssen Pharmaceuticals Inc; Levaquin (levofloxacin) [prescribing information]. February 2017. 37. Alcon; Ciloxan (ciprofloxacin) solution [prescribing information]. March 2006. 38. Allergan. Ocuflox (ofloxacin) [prescribing information]. February 2012. 39. Merus Labs. Factive (gemifloxacin) tablet [prescribing information]. May 2016. 40. Merck & Co. Avelox (moxifloxacin) [prescribing information]. September 2016. 41. Azari AA, Barney NP. Conjunctivitis: A systematic review of diagnosis and treatment. JAMA. 2013;310(16):1721-9. 42. Pfizer Labs. Vibramycin (doxycycline) oral [prescribing information]. August 2014. 43. Alcon. Ciloxan (ciprofloxacin) [prescribing information]. April 2018. 44. Alcon. Tobrex ointment (tobramycin ophthalmic) [prescribing information]. April 2018. 45. Allergan. Polytrim (trimethoprim/polymyxin B) [prescribing information]. August 2004. 46. Allergan. Ocuflox (ofloxacin) [prescribing information]. April 2017. 47. Alcon. Moxeza (moxifloxacin) [prescribing information]. February 2017. |
