 |
A Game Plan for Managing Eyelid Lesions and Related Conditions
Optometrists play a critical role in the identification and treatment of these issues.
By Vera Howe, OD
Jointly provided by the Postgraduate Institute for Medicine (PIM) and the Review Education Group
Release Date: October 15, 2023
Expiration Date: October 15, 2026
Estimated Time to Complete Activity: two hours
Target Audience: This activity is intended for optometrists concerned with skin abnormalities in the ocular area.
Educational Objectives: After completing this activity, participants should be better able to:
Correctly identify various eyelid lesions and conditions in clinical practice.
Effectively manage patients with eyelid lesions.
Recognize when a patient should be referred to a specialist.
Determine when an eyelid lesion may be malignant and requires biopsy.
Disclosure of Conflicts of Interest: PIM requires faculty, planners and others in control of educational content to disclose all their financial relationships with ineligible companies. All identified conflicts of interest are thoroughly vetted and mitigated according to PIM policy. PIM is committed to providing its learners with high-quality, accredited CE activities and related materials that promote improvements or quality in health care and not a specific proprietary business interest of an ineligible company.
Those involved reported the following relevant financial relationships with ineligible entities related to the educational content of this CE activity: Faculty - Dr. Howe have nothing to disclose. Planners and Editorial Staff - PIM has nothing to disclose. The Review Education Group has nothing to disclose.
Accreditation Statement: In support of improving patient care, this activity has been planned and implemented by PIM and the Review Education Group. PIM is jointly accredited by the Accreditation Council for Continuing Medical Education, the Accreditation Council for Pharmacy Education and the American Nurses Credentialing Center to provide CE for the healthcare team. PIM is accredited by COPE to provide CE to optometrists.
Credit Statement: This course is COPE-approved for two hours of CE credit. Activity #126905 and course ID 87274-TD. Check with your local state licensing board to see if this counts toward your CE requirement for relicensure.
Disclosure of Unlabeled Use: This educational activity may contain discussion of published and/or investigational uses of agents that are not indicated by the FDA. The planners of this activity do not recommend the use of any agent outside of the labeled indications. The opinions expressed in the educational activity are those of the faculty and do not necessarily represent the views of the planners. Refer to the official prescribing information for each product for discussion of approved indications, contraindications and warnings.
Disclaimer: Participants have an implied responsibility to use the newly acquired information to enhance patient outcomes and their own professional development. The information presented in this activity is not meant to serve as a guideline for patient management. Any procedures, medications or other courses of diagnosis or treatment discussed or suggested in this activity should not be used by clinicians without evaluation of their patient’s condition(s) and possible contraindications and/or dangers in use, review of any applicable manufacturer’s product information and comparison with recommendations of other authorities.
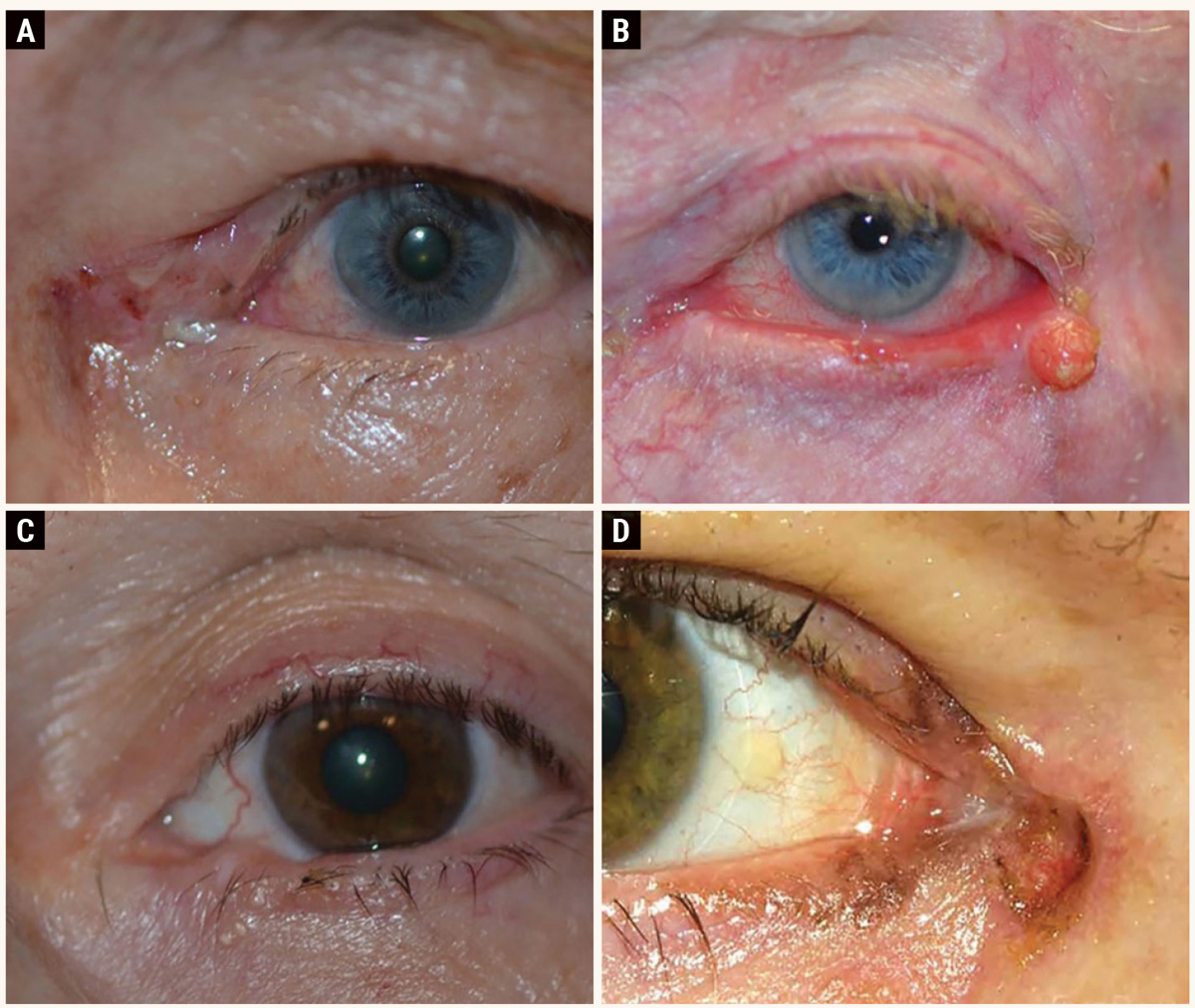 |
This series shows the range of potential eyelid carcinomas: (A) basal cell carcinoma, (B) nodular squamous cell carcinoma, (C) sebaceous cell carcinoma and (D) melanoma. Photos: eyerounds.org, University of Iowa. Click image to enlarge. |
The eyelids are the first structure examined under the slit lamp microscope and are often cursorily evaluated. The eyelids function to protect the front surface of the globes from injury, and the skin is exposed to sunlight and ultraviolet rays. In addition, the eyelids help regulate the amount of light that reaches the eye. The eyelids’ structure is instrumental in tear film maintenance by distributing the tear film over the ocular surface during blinking as well as their action on the conjunctival sac and lacrimal sac in tear flow. Attention to the lids involves examining the dermal surface, the eyelid margins and palpebral conjunctiva as well as the dynamics of lid movement and position as it pertains to the ocular surface and the lacrimal system.
As such, the eyelids are common locations for both benign and malignant lesions to appear and, due to the thin skin and constant use, are prone to age-related changes. Below, the most common lesions and lid malpositions will be reviewed, as well as nonsurgical and pre- and postoperative management.
Eyelid Anatomy
Before you can correctly identify and effectively manage eyelid lesions and conditions, a clear understanding of its anatomy is necessary. The eyelid skin is the thinnest in the body and has no subcutaneous fat. The palpebral conjunctiva is the innermost layer of tissue that lies adjacent to the globe. Anterior to the palpebral conjunctiva is the tarsal plate, the connective tissue structure within the eyelid that provides its rigidity and shape.
Between the tarsal plate and outermost layer of skin is muscle tissue composed of the orbicularis oculi and levator palpebrae superioris. The tarsal plate surrounds and protects the meibomian glands. These glands secrete lipid through openings along the eyelid margin that contributes to the tear film stability. The eyelashes on the eyelid margin are anterior to the meibomian glands and are surrounded by the glands of Moll (apocrine glands) and the glands of Zeis (sebaceous glands).1
Common Eyelid Lesions
The ability to recognize and distinguish between various eyelid lesions is critical for effective patient care. Conditions optometrists will likely encounter in clinical practice include hordeolum, chalazion and pyogenic granulomas, to name a few.
Hordeolum. This is an acute infection associated with an obstructed sebaceous gland, most commonly due to staphylococcus bacteria.1 It appears as a tender, erythematous nodule and can be associated with eyelid edema, superficial skin flaking or crusting or cellulitis or abscess formation. External hordeola are localized infections in the ciliary glands (Zeis or Moll) found at the eyelid margin and appear as a pustule near an eyelash follicle. Internal hordeola occur within the tarsus in the meibomian glands and present with more diffuse tenderness and eyelid erythema.
Hordeola tend to resolve spontaneously, but primary treatment consists of warm compresses multiple times a day. Additional treatment options for hordeola include topical antibiotic ointment, combination antibiotic/steroid ointment and in cases with cellulitis, abscess, or significant inflammation, systemic antibiotics that cover staphylococcal infections (amoxicillin/clavulanate, cephalosporins, fluoroquinolones) may be indicated.2,3 Surgical intervention is not necessary but may be helpful to accelerate resolution.
Chalazion. This focal nodule on the eyelid arises from an obstructed sebaceous gland (meibomian or Zeis). This condition, which affects all age groups, is caused by lipogranulomatous inflammation and may be associated with inflammatory disorders of the eyelid such as rosacea and blepharitis. Chalazia can be treated in the acute phase with warm compresses used for 10 to 15 minutes two to four times daily. Spontaneous resolution can occur about 25% of the time with conservative treatment.4,5
In complex or recurrent cases, oral doxycycline or azithromycin may be considered because of their ability to downregulate the inflammatory cascade, inhibiting bacterial lipase production and improving the tear film balance.6 Surgery or intralesional injection may be indicated in the event of failed conservative management. Intralesional injection is a non-surgical option for recalcitrant chalazia and results in an approximately 80% reduction of the lesion in about two weeks after the first or second injection.5,7 While effective and minimally invasive, appropriate patient selection is imperative as intralesional steroid injections carry the risk of skin depigmentation, dermal and fat atrophy, and intra-arterial embolism, which is a risk with triamcinolone injection.1,5 In the event of chronic or recurrent chalazia, pathologic examination should be performed to rule out masquerade conditions, such as sebaceous cell carcinoma. Intense pulsed light treatment is relatively new in eye care but shows promise as an effective treatment for chalazia.8
Pyogenic granulomas. These non-tender, red, fleshy vascular lesions are often found on skin and mucosa as well as on the palpebral conjunctiva of the eye. They are typically dome-shaped, vary from 1mm to 10mm in diameter and can be pedunculated or sessile. Pyogenic granulomas are vascular lesions that often arise rapidly from an area of insult, such as a hordeolum, chalazion, punctal plug, trauma or surgical site. Most pyogenic granulomas are asymptomatic, but they can bleed easily and cause discomfort.
Removal of the irritant that is responsible for the pyogenic granuloma formation is the first treatment in management; however, pyogenic granulomas rarely resolve spontaneously and require treatment only if they are symptomatic. There is evidence that they respond well to topical therapies, such as corticosteroids or beta blockers.9,10 Topical steroids should be used four times a day for one to two weeks or topical beta blockers, such as timolol maleate 0.5% twice daily for at least three weeks. Beta blockers can be remarkably effective and do not carry the risk of steroid-induced intraocular pressure response.11 In cases where there is not effective resolution of the lesion, surgical excision remains an option.
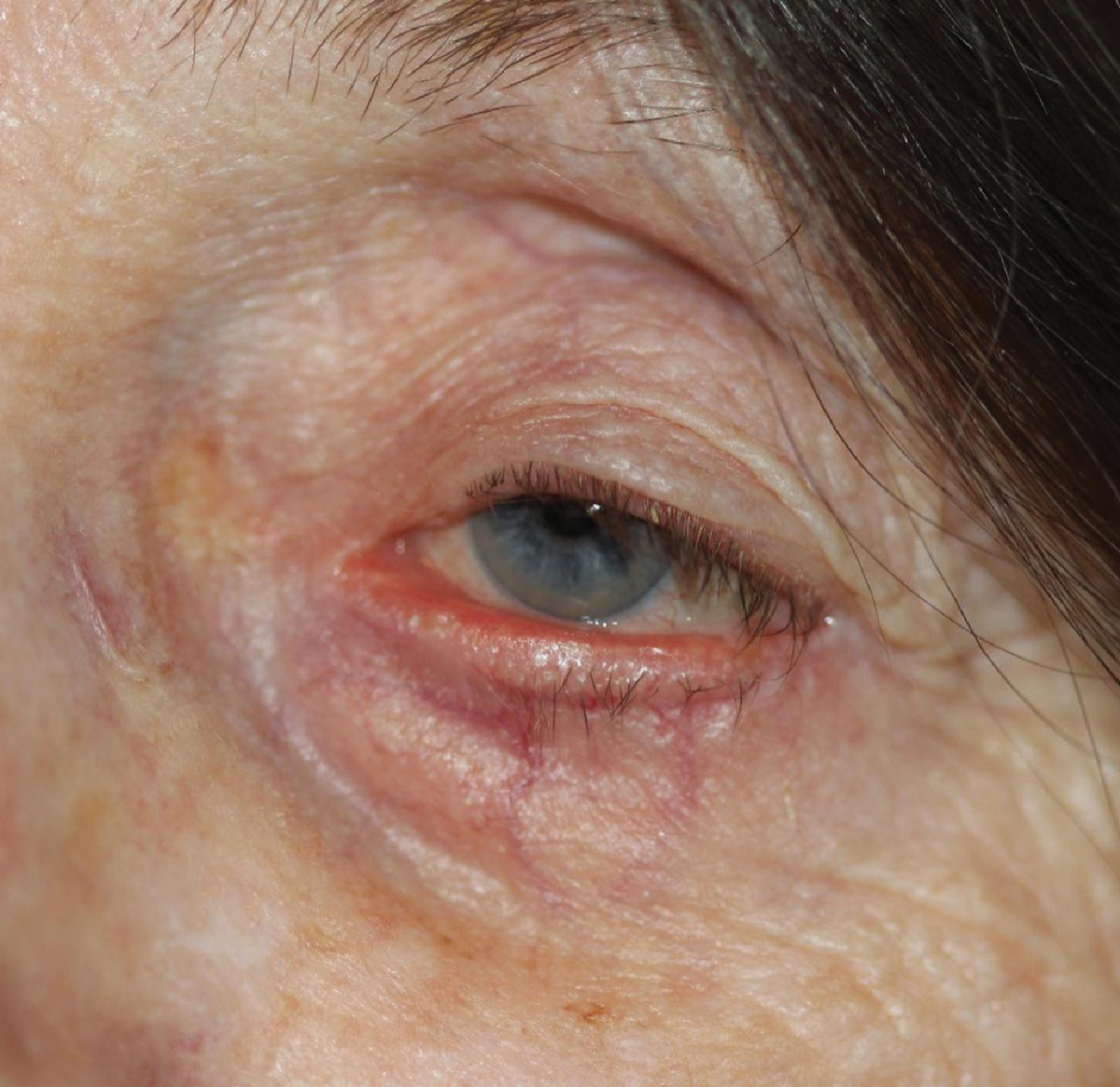
 |
|
Bilateral lid ptosis. The margin reflex distance (MRD) 1 is -1mm. Click image to enlarge. |
Malignant Eyelid Lesions
The most common malignant eyelid lesions are basal cell carcinoma, squamous cell carcinoma and sebaceous cell carcinoma.12 Less commonly, melanoma can be identified. Eyelid malignancies have common characteristics of ulceration, a chronic, nonhealing lesion, intermittent bleeding, asymmetric appearance, madarosis and destruction of the normal eyelid anatomy. Any lesion that is suspicious should be biopsied and sent for histologic evaluation.
Basal cell carcinoma (BCC). The most common eyelid malignancy, basal cell carcinoma accounts for approximately 90% to 95% of malignant eye tumors in the United States.2 They are found most often on sun exposed eyelid skin, most commonly the lower eyelid and medial canthus. Nodular BCC is the most common form, and these lesions have a pearly border with telangiectasias and tend to ulcerate. Morpheaform BCC is less common but more aggressive than nodular BCC. The morpheaform BCC lesion tends to be firm and slightly elevated and have indeterminate margins. Patients at highest risk for basal cell carcinoma are fair-skinned, blue-eyed, blonde, or red-haired, middle aged or older, and with British or Scandinavian ancestry.2,13 Treatment depends on size and location and can include surgical excision, topical immunotherapy, radiotherapy and oral treatment. Surgical excision is considered the gold standard of treatment, which includes Mohs microangiographic surgery and frozen section evaluation. For individuals in which surgery alone is not possible, these other treatments have had varying levels of success. 13
Squamous cell carcinoma (SCC). This condition accounts for 5% to 10% of eyelid malignancies and is more aggressive than BCCs. SCCs is often found on lower and upper eyelids and the medial canthus but may be present on more than one periocular area and appear as elevated, nonhealing, erythematous lesions.14 They tend to have a flaky appearance, caused by the production of keratin as they arise from keratinocyte proliferation. The lesion may arise spontaneously or from areas of solar injury or actinic keratosis. SCC may invade into orbit or intracranially. Risk factors include male gender, fair complexion, history of ultraviolet exposure, a high fat diet, chemical exposure, smoking and immunosuppression.12 Individuals who are immunocompromised are more prone to aggressive SCCs. Treatment is complete excision with histological confirmation of clear margins, although for individuals who are not good surgical candidates, targeted epidermal growth factor receptor (EGFR) has shown promise.12 In the event of orbital invasion, exenteration may be required.
Sebaceous cell carcinoma (SebCCa). This highly malignant and potentially lethal tumor arises from the oil glands of the eyelid, namely meibomian and Zeis glands or the sebaceous glands of the caruncle, eyebrow or facial skin. It occurs evenly in men and women and occurs twice as frequently in the upper lid as it does in the lower lid due to a greater number of sebaceous glands in the upper lids.2,15 SebCCa is the most common eyelid malignancy in the Asian-Indian population, and the third most common in the Caucasian population.12,16 SebCCa occurs primarily in those over the age of 50, with the greatest incidence among those in their 70s and 80s. It is known as the “great masquerader” as it may present as chronic unilateral blepharoconjunctivitis or chronic or non-healing chalazion. A hallmark feature of SebCCa is pagetoid spread and skip lesions, so wide excision of the primary lesion and map biopsies (this includes the palpebral conjunctiva in the superior and inferior lids as well multiple sections of the bulbar conjunctiva) must be performed.17 Surgical excision is the primary treatment method for SebCC. A fresh tissue histology is necessary to establish clear margins due to the malignant nature of sebaceous cell carcinoma.12,17
Primary melanoma of the eyelid skin. While this is a rare entity (<0.1% of eyelid malignancies), the incidence of melanoma in the United States has steadily increased over the last 30 years. Melanomas typically have variable pigmentation and irregular borders and may ulcerate and bleed. Melanoma risk factors include sun exposure, tanning bed use, genetic predisposition and environmental mutagens.2 Melanoma should be suspected in any patient over the age of 20 with an acquired pigmented lesion. Primary treatment of a melanoma skin lesion on the eyelid includes wide excision with histologic confirmation of complete tumor removal.2,18
 |
|
Bilateral upper lid dermatochalasis. The upper lids are resting on the eyelashes, causing downward misdirection. Click image to enlarge. |
Eyelid Malpositions
Patients with eyelid malpositions require careful evaluation with a focus on general medical history and eyelid condition history. Careful attention should be paid to visual acuity, pupil function, extraocular muscles, ocular surface and tear layer. External photography and visual field examination are also helpful. Malpositions of the eyelids can affect the upper and lower eyelids. The most common eyelid malpositions are upper eyelid ptosis and dermatochalasis as well as lower eyelid ectropion and entropion.
Ptosis. Upper eyelid ptosis can be due to ptosis (the actual eyelid margin being low) or due to dermatochalasis (redundant upper eyelid skin). Both ptosis and dermatochalasis can limit a patient’s visual field or activities of daily living.
Ptosis is classified as either congenital or acquired, and further described as myogenic, involutional, mechanical or neurogenic. Congenital ptosis in a small child can result in amblyopia. The most common cause for acquired ptosis is involutional (age-related) and is due to the stretching of the aponeurosis of the levator muscle. This can also be caused by repetitive traction on the eyelid, such as with eye rubbing or prolonged use of contact lenses, or by previous eyelid surgery or intraocular surgery. In this condition, the strength of the levator muscle remains normal. Clinical findings will often include ptosis that is worse on downgaze and elevation of the eyelid crease, and the patient will often complain of ptosis that makes reading more difficult.19
Clinical evaluation of ptosis includes a detailed history, which can provide details regarding variability and time frame. Photographs are helpful in establishing a timeline regarding onset of ptosis, while family history can bring attention to inherited conditions. Examination of the ptosis patient can include the following clinical measurements: margin reflex distance (MRD) 1 and 2, palpebral fissure height, upper eyelid crease position, levator function and presence of lagophthalmos or punctate epithelial erosions. To determine how the ptosis affects function, head position, chin elevation, brow position and brow action in attempted up gaze needs to be evaluated. Pupil examination is also necessary, particularly in unilateral cases, to rule out associated conditions such as Horner’s syndrome (miosis in dim illuminations) and cranial nerve III palsy (which may have mydriasis and exotropia). Additionally, a visual field will quantify the level of functional visual field loss and can be used to demonstrate to insurance companies the improvement in visual field with the upper lid taped. Full face photography is often included.
Management of ptosis is as varied as its causes. Care must be taken to determine whether repair will be functional or cosmetic. Functional repairs would be those that could cause amblyopia, have significant superior visual field loss or cause difficulty with reading. Non-surgical options include temporary ptosis correction with a variety of medications. Botulinum toxin can be injected to weaken the upper lid orbicularis and provides improvement lasting about three months. Apraclonidine can be used up to three times daily to provide some improvement as an alpha 2 agonist. Tetrahydrozoline is a non-selective alpha agonist and can provide mild lid elevation, but frequent use should be cautioned against due to ocular surface side effects. Recently, the US FDA approved 0.1% oxymetazoline hydrochloride ophthalmic solution for temporary ptosis improvement, which can maintain 1mm to 2 mm of lid elevation for six to 14 hours. Ptosis eyelid crutches mounted on eyeglass frames can be used for those with severe ptosis in individuals that cannot undergo surgical repair. The type of surgical repair for ptosis is dependent on the function of the levator muscle. In the presence of good levator function, an external approach with levator advancement or internal repair with conjunctival muellerectomy are indicated. An internal approach (frontalis sling) may be indicated for individuals with poor levator function.20
The most common complication of surgical ptosis repair is under correction. In the early postoperative period, it is important to differentiate this from eyelid edema causing mechanical ptosis. Other complications include overcorrection, wound healing complications, uneven eyelid height, unacceptable eyelid contour, conjunctival prolapse, tarsal eversion, contralateral ptosis or lagophthalmos with exposure keratopathy.2
 |
|
This patient presents with epiphora due to involutional ectropion and loss of punctal apposition to the globe. Click image to enlarge. |
Dermatochalasis. This is redundancy of eyelid skin, often associated with fat pad prolapse (steatoblepharon) and may accompany ptosis. While more common in the elderly, it can be found in middle-aged individuals with a family history.19 Individuals with upper eyelid dermatochalasis may complain of a heavy feeling around their eyes, brow ache, perceiving their upper eyelashes in their field of vision and reduction in their visual field, particularly superiorly. Patients often complain that their upper eyelid skin rubs their eyelashes, and report difficulty wearing mascara due to smearing. The effects of dermatochalasis may be made worse when accompanied by brow ptosis. Lower eyelid dermatochalasis is considered cosmetic by most third-party payers.
Upper eyelid blepharoplasty was the second most performed procedure in the US in 2020.21 This procedure is commonly sought after to improve function by removing excess skin, muscle and/or fat which can obstruct the superior visual field. Upper eyelid blepharoplasty can also be performed to improve appearance. Lower lid blepharoplasty is performed for cosmetic indications. Aggressive resection of lower eyelid skin and fat may lead to eyelid retraction, ectropion or a sunken periorbital appearance.2
The evaluation for blepharoplasty includes a complete examination of the ocular structures and visual acuity, a history with attention to previous periocular surgeries, careful documentation of the amount and areas of redundant eyelid tissue and prolapsed fat in both the upper and lower eyelids, presence of lagophthalmos and tear film evaluation and external photography. Prior to surgical referral, dry eye therapy should be maximized, with frequent use of artificial tears, thicker nighttime lubricants and potentially punctal plug placement, as postoperative dryness is quite common. Additionally, upper blepharoplasty evaluation includes visual field testing, evaluation of forehead and brow height and contour to assess the presence of brow ptosis and the assessment of the upper eyelid crease. Evaluation may include photographs of the brow and eyelids. Lower lid blepharoplasty includes assessment of lower lid elasticity and notation of the orbital rims to avoid postoperative scleral show.
In the immediate postoperative period, management is aimed at improving comfort. Icing the lids helps reduce edema and bruising, but it is normal to expect dry eye symptoms in the first two weeks after a blepharoplasty, as there is reduction in orbicularis function from both edema and anesthetic. Immediately after surgery, the patient will be directed to use ointment, but in subsequent weeks, dryness from post-surgical blink dynamic is common. Serious complications in the post-operative period include orbital hemorrhage, diplopia, excess removal of skin and very rarely, loss of vision.2
The patient should be monitored for significant pain, marked asymmetric swelling or new proptosis. Dimming of vision or asymmetric blurred vision should be evaluated immediately for orbital hemorrhage. Individuals with hypertension, blood dyscrasias and those on anticoagulants are most at risk for hemorrhage. Diplopia can arise due to injury to the trochlea of the superior oblique muscle in upper lid blepharoplasty or to the inferior oblique or inferior rectus in lower lid blepharoplasty. Excess removal of skin can result in lagophthalmos of the upper eyelid as well as eyelid retraction or cicatricial ectropion.2
Lateral canthal tendon disinsertion (LCTD). This condition results in a change from the normal eyelid fissure symmetry, blink dynamics and lacrimal pump function.22 LCTD is often the cause of persistent discharge, ocular irritation and epiphora. The clinical examination demonstrates medial and inferior movement of the lateral commissure with attempts at eyelid closure, lack of apposition of the eyelid margin with associated corneal exposure and a vertically displaced lateral canthal angle.
Additionally, narrowing of the horizontal palpebral fissure, temporal overlap of the eyelids on attempted closure and pseudo upper or lower eyelid retraction is often observed. Clinical exam can confirm the diagnosis by using a cotton-tipped swab to physically reposition the lateral canthal angle temporally and toward the orbit, confirming the diagnosis of LCTD. Surgical repair options include lateral canthopexy, lateral canthoplasty or lateral tarsorrhaphy.22
Floppy eyelid syndrome. This condition is characterized by ocular irritation, conjunctival injection, eyelash ptosis and mild mucus discharge that is worse on awakening.23 Patients will often have chronic papillary conjunctivitis and a superior tarsal plate that is rubbery and easily everted. During the exam, the lax upper eyelid may evert spontaneously, especially when pulled up toward the forehead. Often these patients are stomach sleepers, with the pillow causing mechanical upper lid eversion and irritation of the superior conjunctiva by the bedding. Floppy eyelid syndrome is associated with obesity, obstructive sleep apnea, keratoconus, eyelid rubbing and hyperglycemia.23 Treatment begins with conservative medical management, viscous lubrication with lid taping or a shield use at night. If the patient has sleep apnea, use of CPAP may reduce face down sleep positioning. Surgical correction in the form of wedge resection is indicated if refractory to other treatments.
Ectropion. This condition may be classified as congenital, involutional, cicatricial, paralytic or mechanical. Most cases of ectropion are involutional, arising from horizontal eyelid laxity in the medial or lateral canthal tendons or both. This results in loss of apposition of the eyelid to the globe and the eyelid margin is everted. The conjunctival surface can become chronically inflamed and keratinized due to mechanical irritation and drying of the surface of the conjunctiva. Most cases of involutional inferior ectropion occur due to the effects of gravity on a lax lower lid. Cicatricial ectropion occurs due to a deficiency of skin, which may be due to thermal or chemical burns, mechanical injury, aggressive lid surgery or chronic actinic skin damage. Numerous conditions that result in chronic skin inflammation such as rosacea, atopic dermatitis, eczematoid dermatitis or scarring from herpes zoster can cause cicatricial ectropion. Paralytic ectropion is usually due to CN VII paralysis or palsy. Mechanical causes of ectropion include large eyelid masses, fluid accumulation, or herniated orbital fat. Congenital ectropion is rarely an isolated finding and is often associated with chromosomal abnormalities.2
When evaluating the lower lid, attention must be paid to the punctal position and assessing lid laxity. The distraction test and snapback test are used to assess this. The distraction test is performed by grasping the lower lid and pulling it away from the globe. If the eyelid can be pulled more than 10mm from the globe, it is considered to have significant lid laxity. Additionally, the snapback test is performed by pulling the lower lid down and away from the globe. The lid is held in position for several seconds, and then released.24 The amount of time it takes the lid to return to its original location and is graded on a scale from 0 (immediately returns to original position) to IV (never returns). If a blink is required to return the lid to its original position, it is grade III.
Treatment for ectropion depends on the underlying cause. Medical management of ectropion is targeted at protecting the ocular surface and includes lubrication with both drops and ointments, taping the lower lid temporally or even moisture chamber goggles. Surgical repair depends on the degree of ectropion and corneal surface health indicated for involutional ectropion. Cicatricial ectropion includes medical management of the underlying cause, protection of the corneal and conjunctival surfaces, and often surgical intervention. Mechanical ectropion is treated by addressing the underlying cause.
 |
|
This patient suffers from corneal irritation resulting from trichiasis caused by lower lid entropion. Click image to enlarge. |
Entropion. This can occur in the upper or lower eyelids, is found unilaterally or bilaterally and is classified as congenital, involutional, acute spastic and cicatricial. Most patients will have complaints of tearing, foreign body sensation, irritation and chronic red eye. The most common cause of lower lid entropion is involutional, which is the result of horizontal eyelid laxity, attenuation or disinsertion of eyelid retractors and overaction of the preseptal orbicularis oculi muscle. Horizontal eyelid laxity is a consequence of aging, characterized by the stretching of the tendons of the eyelid and canthus. Attenuation of the eyelid retractors combined with preseptal orbicularis overaction results in inward rotation of the lid margin. Cicatricial entropion is due to contracture of the palpebral conjunctiva, which cause the eyelid to rotate inward. Several conditions can lead to scarring, including autoimmune, inflammatory, infectious, surgically-induced and traumatic conditions.
Additionally, long term use of topical glaucoma medications, especially miotics and prostaglandins can cause chronic conjunctivitis with conjunctival shortening and secondary cicatricial entropion. On clinical examination, if it is possible to manually place the eyelid in its normal anatomic position, the cause is involutional rather than cicatricial. Acute spastic entropion can be a result of chronic ocular irritation or inflammation that results in contraction of the orbicularis oculi muscle that causes inward rotation of the eyelid margin. The chronic corneal irritation from the entropion perpetuates the cycle of orbicularis spasm.2
Treatment of involutional entropion is first achieved with lubrication, appropriate eyelid taping and bandage contact lens. If this treatment is inadequate, surgical repair is necessary. Acute spastic entropion will often resolve when the underlying cause is effectively treated. Temporary relief can often be obtained with taping of the eyelid to evert the lid margin, cautery or rotational suture placement. In some cases, botulinum toxin can be used to paralyze the preseptal orbicularis muscle.
Management of cicatricial entropion depends on the underlying cause. Surgery is often required, but lubrication, bandage contact lenses and removal of trichiatic lashes can be helpful. Surgery is not indicated during periods of exacerbation of autoimmune disease or until stabilization of an acute inflammatory illness. Congenital entropion tends not to resolve spontaneously and may require surgical correction.25
Takeaways
As primary eyecare providers, the role optometrists play in the identification, treatment and management of eyelid lesions and conditions is enormous. Optometrists can identify and treat many eyelid lesions and are instrumental in referring malignancies to our surgical colleagues when needed. Accurate assessments of common eyelid conditions and appropriate medical management can improve the quality of life of our patients and may delay or eliminate the need for surgery. Proper presurgical assessments can ensure that surgical candidate selection is optimized, resulting in ideal postoperative results.
Dr. Howe is a clinical assistant professor at the University of Iowa Hospitals and Clinics Department of Ophthalmology and Visual Sciences in Iowa City, IA, where she serves as the director of Optometric Services. She graduated from the Illinois College of Optometry and completed her contact lens and cornea residency at the Illinois Eye Institute. She is a fellow of the American Academy of Optometry. She has no financial interests to disclose.
1. Skorin L, Goemann L. Eyelid inflammation: approach to hordeolum, chalazion and pyogenic granuloma. Consultant. 2017;57(5):282-5. 2. Korn BS. 07, Oculofacial plastic and orbital surgery [online course]. American Academy of Ophthalmology 2022-2023 Basic and Clinical Science Course. Accessed August 15, 2023. 3. Alsoudi AF, Ton L, Ashraf DC, et al. Efficacy of care and antibiotic use for chalazia and hordeola. Eye Contact Lens. 2022;48(4):162-8. 4. Wu AY, Gervasio KA, Gergoudis KN, et al. Conservative therapy for chalazia: is it really effective? Acta Ophthalmol. 2018;96(4):e503-9. 5. Perry HD, Serniuk RA. Conservative treatment of chalazia. Ophthalmology. 1980;87(3):218-21. 6. Wladis EJ, Bradley EA, Bilyk JR, et al. Oral antibiotics for meibomian gland-related ocular surface disease: a report by the American Academy of Ophthalmology. Ophthalmology. 2016;123(3):492-6. 7. Mohan K, Dhir SP, Munjal VP, et al. The use of intralesional steroids in the treatment of chalazion. Ann Ophthalmol. 1986;18(4):158-60. 8. Caravaca A, Alio Del Barrio JL, Martinez Hergueta MC, Amesty MA. Intense pulsed light combined with meibomian gland expression for chalazion management. Arch Soc Esp Oftalmol (Engl Ed). 2022;97(9):490-6. 9. Oke I, Alkharashi M, Petersen RA, et al. Treatment of ocular pyogenic granuloma with topical timolol. JAMA Ophthalmol. 2017;135(4):383-5. 10. Ferry AP. Pyogenic granulomas of the eye and ocular adnexa: a study of 100 cases. Trans Am Ophthalmol Soc. 1989;87:327-43; discussion 343-7. 11. DeMaria LN, Silverman NK, Shinder R. Ophthalmic pyogenic granulomas treated with topical timolol-clinical features of 17 cases. Ophthalmic Plast Reconstr Surg. 2018;34(6):579-82. 12. Yin VT, Merritt HA, Sniegowski M, et al. Eyelid and ocular surface carcinoma: diagnosis and management. Clin Dermatol. 2015;33(2):159-69. 13. Shi Y, Jia R, Fan X. Ocular basal cell carcinoma: a brief literature review of clinical diagnosis and treatment. Onco Targets Ther. 2017;10:2483-9. 14. Faustina M, Diba R, Ahmadi MA, et al. Patterns of regional and distant metastasis in patients with eyelid and periocular squamous cell carcinoma. Ophthalmology. 2004;111(10):1930-2. 15. Dasgupta T, Wilson LD, Yu JB. A retrospective review of 1349 cases of sebaceous carcinoma. Cancer. 2009;115(1):158-65. 16. Patel BCK. Epidemiology of eyelid malignancies in indian asians: the importance of being earnest. Ocul Oncol Pathol. 2019;5(3):205-9. 17. Song A, Carter KD, Syed NA, et al. Sebaceous cell carcinoma of the ocular adnexa: clinical presentations, histopathology, and outcomes. Ophthalmic Plast Reconstr Surg. 2008;24(3):194-200. 18. Chan FM, O’Donnell BA, Whitehead K, et al. Treatment and outcomes of malignant melanoma of the eyelid: a review of 29 cases in Australia. Ophthalmology. 2007;114(1):187-92. 19. Allen RC, Harper RA. Basic ophthalmology: essentials for medical students, 10th edition. American Academy of Ophthalmology. 2016. 20. Cahill KV, Bradley EA, Meyer DR, et al. Functional indications for upper eyelid ptosis and blepharoplasty surgery: a report by the American Academy of Ophthalmology. Ophthalmology. 2011;118(12):2510-7. 21. Surgeons ASoP. Plastic Surgery Statistics Report. ASPS. www.plasticsurgery.org/documents/News/Statistics/2020/plastic-surgery-statistics-full-report-2020.pdf. Accessed 15 August 2023. 22. Shriver EM, Erickson BP, Kossler AL, et al. Lateral canthal tendon disinsertion: clinical characteristics and anatomical correlates. Ophthalmic Plast Reconstr Surg. 2016;32(5):378-85. 23. Skorin L, Jr., Knutson R. Ophthalmic Diseases in Patients With Obstructive Sleep Apnea. J Am Osteopath Assoc. 2016;116(8):522-9. 24. Skorin L, Jr., Lange R. Ectropion: classification, diagnosis and management. Consultant. 2108;58(6):e180. 25. Skorin L, Jr. A review of entropion and its management. Cont Lens Anterior Eye. 2003;26(2):95-100. |
