 |
When Your Patient Complains of Red Eye
The key to uncovering the root cause is a thorough patient history and clinical exam.
By Suzanne Sherman, OD, and Christina Cherny, OD
Release Date: November 15, 2021
Expiration Date: November 15, 2024
Estimated Time to Complete Activity: 2 hours
Jointly provided by Postgraduate Institute for Medicine (PIM) and Review Education Group
Educational Objectives: After completing this activity, the participant should be better able to:
- Discuss the pathophysiology behind red eye.
- Conduct a careful and comprehensive patient history.
- Recognize what to look for during the clinical exam.
- Identify and diagnose the underlying cause of the red eye.
Target Audience: This activity is intended for optometrists engaged in managing patients who present with red eye.
Accreditation Statement: In support of improving patient care, this activity has been planned and implemented by the Postgraduate Institute for Medicine and Review Education Group. Postgraduate Institute for Medicine is jointly accredited by the Accreditation Council for Continuing Medical Education, the Accreditation Council for Pharmacy Education, and the American Nurses Credentialing Center, to provide continuing education for the healthcare team. Postgraduate Institute for Medicine is accredited by COPE to provide continuing education to optometrists.
Reviewed by: Salus University, Elkins Park, PA
Faculty/Editorial Board: Suzanne Sherman, OD, and Christina Cherny, OD
Credit Statement: This course is COPE approved for 2 hours of CE credit. Activity #122799 and course ID 75278-GO. Check with your local state licensing board to see if this counts toward your CE requirement for relicensure.
Disclosure Statements:
Authors: Drs. Sherman and Cherny have no financial interests to disclose.
Managers and Editorial Staff: The PIM planners and managers have nothing to disclose. The Review Education Group planners, managers and editorial staff have nothing to disclose.
A “red eye” is one of the most common clinical signs and symptoms encountered in eye care. A variety of etiologies exist, making the clinical history an important component in narrowing down the list of differential diagnoses. A thorough examination of clinical signs and symptoms is necessary to appropriately diagnose and manage these patients.
Red eye is a broad term, encompassing anything from the garden variety viral infection to allergic reactions, or a vision-threatening infection. This article will discuss the pathophysiology behind the red eye and how to take a careful ocular, medical and social history from the patient. We will also delve into what to look for during the exam to find clues that will lead to the underlying cause and how to proceed accordingly.
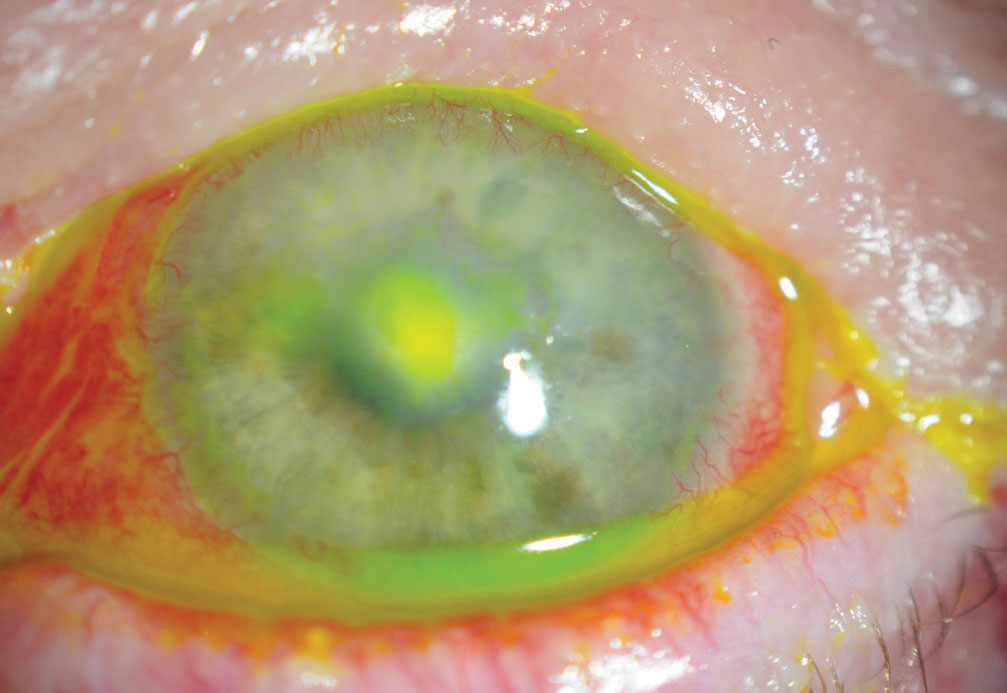 |
| This neurotrophic cornea developed a bacterial ulcer. The patient came in acutely due to redness but was not in any pain. Click image to enlarge. |
Clinical History and Exam
A systematic approach to patient history and clinical examination is key in properly managing each patient who presents with a red eye. Topics to ask the patient about include laterality, symptom duration and course, rapid or gradual onset, quality and quantity of discharge, presence of diffuse or sectoral hyperemia, pain, photophobia, decreased vision, prior or concurrent medical or topical treatment, contact lens use, allergies, systemic disease, previous trauma and surgical and social history.1 As data is collected during the exam, a working diagnosis should begin to form, along with several alternative differentials.
Conditions With Mild to Moderate Pain
Patients can present with red eye due to any number of problems, from contact lens discomfort and allergies to episcleritis, conjunctivitis and dry eye, to name a few. The many causes of red eye are associated with varying levels of discomfort and pain. To ensure an appropriate diagnosis and treatment, optometrists must have the knowledge to differentiate these various conditions:
Conjunctivitis. The most common cause of red eye symptoms, this condition is an inflammation of the bulbar and palpebral conjunctiva.1 Inflammation of the conjunctiva is precipitated by infectious pathogens, noninfectious irritants and dryness.1-4 This leads to injection or dilation of the conjunctival vessels, resulting in the characteristic hyperemia and edema seen in conjunctivitis.4 Additional symptoms include a mild burning sensation, epiphora and discharge.2,4 Minimal pain and photophobia are expected. Visual acuity, pupils and the anterior chamber are typically unaffected, and sodium fluorescein uptake is not expected.2 Noninfectious etiologies include allergies or ocular irritants; causative agents may vary seasonally.1,2 Infectious etiologies include viral and bacterial organisms and are typically self-limiting, although topical treatment may be administered in many cases to help speed up resolution or prevent secondary infection.
Viral conjunctivitis. Viral infection is the most predominant conjunctivitis etiology. Viral conjunctivitis typically presents with watery discharge in the setting of a hyperemic eye.1-3 An upper respiratory infection may precede ocular symptoms, and preauricular lymph nodes may be enlarged.1-3
The peak season for common variety strains of viral conjunctivitis is in the summer.3 The most common causative pathogen is the adenovirus, and spontaneous resolution of signs and symptoms often occurs within one to two weeks.1-3 Due to the highly contagious nature that persists one to two weeks from onset, contact precautions and hygiene are necessary, and sterilization of exam rooms is imperative after each patient encounter.1,2 Treatment for viral infections includes supportive care with preservative-free artificial tears up to eight times per day, which can be cooled for added comfort, as well as cold compresses and ocular decongestants.1
In cases of viral keratitis secondary to herpetic infections as well as epidemic keratoconjunctivitis (EKC) strains, pain and photophobia may be present.5 A betadine rinse may be useful early on in an EKC infection to reduce the viral load and expedite healing. Furthermore, care must be taken in EKC infections to remove pseudomembranes every few days to prevent symblepharon formation, with lid eversion performed at each visit to detect superiorly located pseudomembranes.
Herpetic infections due to the varicella zoster virus (VZV) may be preceded by vesicular facial lesions along the V1 distribution of the trigeminal nerve.5 Corneal signs may include pseudodendritic epithelial defects in VZV caused by nerve inflammation (referred to as metaherpetic keratopathy), while true branching dendrites with terminal bulbs are apparent in herpes simplex infections (shedding viral particles, referred to as dendritiform keratopathy). Viral conjunctivitis infections caused by the herpes family of viruses are not as likely to spread as common strains.1,2 Herpetic ocular infections are treated with systemic and topical antivirals, although topical steroids may also be indicated in certain cases (so long as they are used concurrently with topical antivirals).5 Metaherpetic keratopathy is often treated with topical antibiotic drops or ointments. Referral to ophthalmology is warranted in cases that do not resolve after a week as well as in suspected herpetic cases.1
Bacterial conjunctivitis. This condition secondary to common causative organisms typically presents with mucopurulent discharge and bilateral matting/crusting of the eyelashes, as well as a lack of prior conjunctivitis and itching.2 However, bacterial conjunctivitis due to Neisseria gonorrhoeae is responsible for a sudden, hyperacute presentation and is associated with profuse mucopurulent discharge, pain, corneal perforation and vision loss.1,2
Signs and symptoms of acute bacterial conjunctivitis generally persist for less than four weeks and are self-limiting, although topical antibiotics may shorten duration.1-3 Bacterial conjunctivitis is considered highly contagious and spreads through direct contact with infected objects.1 This condition most commonly occurs during the winter season.3 Causative organisms are often Staphylococcus aureus in adults and Streptococcus pneumoniae and Haemophilus influenza in children, although cases of Chlamydia trachomatis, diphtheria and Neisseria gonorrhea can also be seen.1-3 Treatment for gonococcal conjunctivitis consists of intravenous ceftriaxone, and concurrent treatment of chlamydial conjunctivitis is necessary.2 Systemic testing for sexually transmitted infections may be indicated for the patient, as well as for their partner(s).
In cases of chronic bacterial conjunctivitis, signs and symptoms may last a minimum of four weeks and can repeatedly relapse.1 When conjunctivitis signs and symptoms are refractory to standard antibiotic treatment, chlamydial conjunctivitis should be considered, particularly if a chronic follicular response is present.1 Other characteristic features include an Arlt’s line on the superior palpebral conjunctiva as well as Herbert’s pits along the superior limbus. Treatment includes topical erythromycin ointment, a single dose of oral azithromycin or a two-week course of doxycycline, as well as treatment of sexual partners. Prompt ophthalmology referral is necessary in cases of suspected gonococcal conjunctivitis and chronic bacterial conjunctivitis, particularly if the patient is refractory to therapy.1
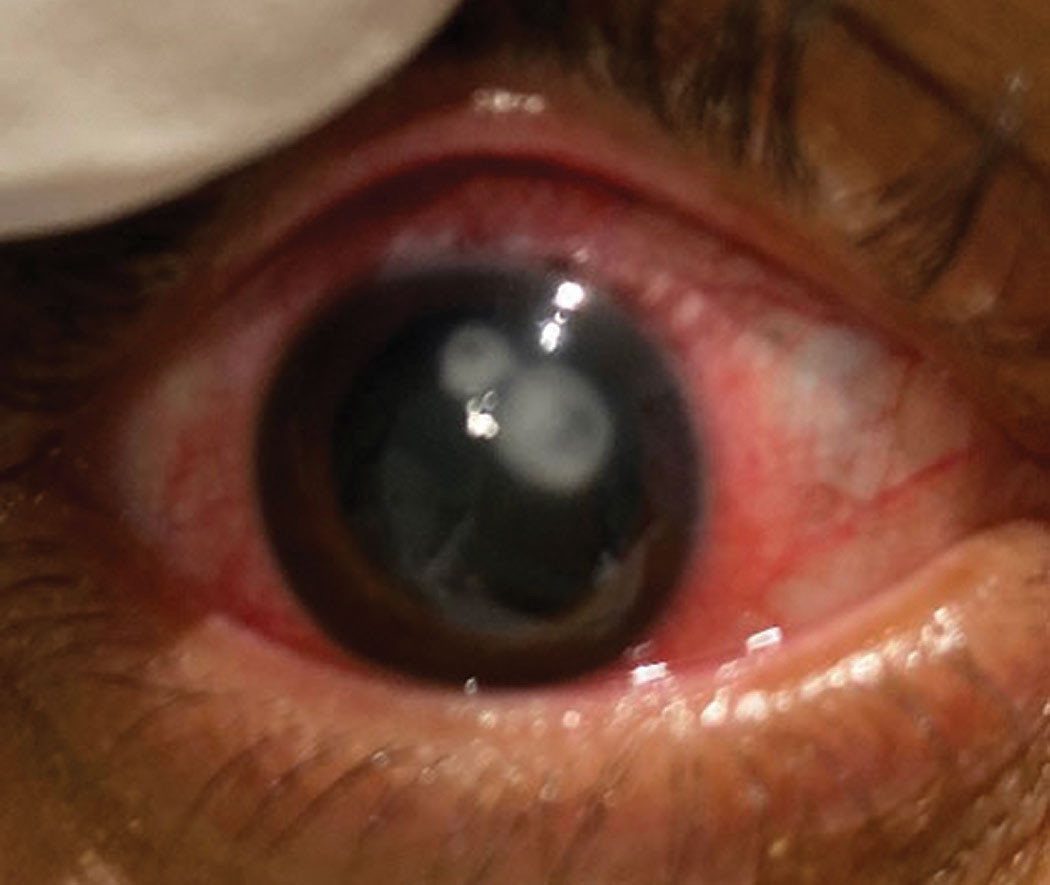 |
| This patient has a presumed Pseudomonas ulcer. Click image to enlarge. |
Allergic conjunctivitis. This typically presents with symptoms of itching and eye rubbing.1,3 It occurs in 25% of the United States population and is associated with atopic disease, including rhinitis, asthma and eczema.1 Allergic conjunctivitis can be season-specific or perennial, which continues throughout the year.1 The seasons most often associated with allergic conjunctivitis are spring and summer (vernal or catarrhal conjunctivitis).3 Avoidance of a patient’s allergen(s) is recommended to alleviate symptoms.1,3 Additional treatment options include over-the-counter antihistamine or vasoconstrictor drops, prescription anti-allergy drops, such as topical histamine H1 receptor antagonists, mast cell stabilizers and combinations, and mild topical steroids in severe cases.1,2 Avoidance of eye rubbing should be stressed, as this has been associated with the development of keratoconus, an ectatic corneal condition.6
Blepharitis. This inflammation of the eyelids may be accompanied by flaking, seborrheic dermatitis and obstructed meibomian gland orifices, as well as redness of the nose and/or cheeks in cases of rosacea.1,7 Anterior blepharitis involves the eyelashes and is often considered to be infectious, caused by bacterial, viral or parasitic agents, while posterior blepharitis involves the meibomian glands and is considered metabolic.8 Treatment of blepharitis generally begins with long-term eyelid hygiene including eye scrubs, lid massage and warm compress application.1,8 In more severe cases, topical ophthalmic antibiotics or steroid/antibiotic combinations may be considered. Meibomian gland dysfunction often requires the addition of oral antibiotics such as doxycycline or tetracycline.1,8 If Demodex mites are present, green tea tree oil and oral ivermectin may be used in addition to lid hygiene.9
Dry eye. Also known as keratoconjunctivitis sicca, this is a commonly encountered ocular condition that occurs due to poor quality or decreased quantity of the tear film.1 Patients may present with complaints of dryness, burning, tearing, stinging, grittiness photophobia and redness.1,7,9 Some patients experience symptoms that are worse than signs, while others present with significant clinical signs and abnormal diagnostic testing despite minimal symptomology.1,9 Conjunctival hyperemia in the setting of dry eye has a non-specific pathophysiology, generally stemming from concurrent conjunctival inflammation.10 This hyperemia may be worsened by topical over-the-counter vasoconstrictor use, which temporarily decreases redness by constricting episcleral vasculature but ultimately results in a rebound effect and further hyperemia.10
Characteristic signs of dry eye include punctate epitheliopathy, meibomian gland dysfunction and a short tear breakup time, among others.9 Risk factors for dry eye include older age and female gender, as well as certain underlying systemic conditions and medications.1 While dry eye diagnosis is often made based on clinical findings, diagnostic tests can be used to further classify the condition, including Schirmer, phenol red, tear osmolarity and inflammatory biomarker testing.9
Treatment of dry eye varies based on etiology (evaporative, tear quantity, mucus deficiency), as well as on severity of signs and symptoms. The initial treatment modality usually begins with frequent ocular lubrication, such as daily instillation of artificial tears and gel drops or ointments at bedtime.1 Preservative-free, single-use formulations are often beneficial to minimize the risk of further dryness or irritation.1 In more advanced dry eye cases, topical ophthalmic treatment with cyclosporine, lifitegrast, corticosteroids or autologous serum tears may be necessary.1,9 Additional treatments include meibomian gland expression (via application of heat or manual expression), humidifiers, eye shield goggles, punctal occlusion or cautery, systemic omega-3 fatty acid therapy and oral doxycycline.1,9
Carotid-cavernous sinus fistula. This occurs when an abnormal communication is formed between the internal carotid artery and the cavernous sinus, and can be direct or indirect (dural).5,11 This may result in tortuous dilatation of the conjunctival and episcleral vessels, leading to a significant hyperemic appearance to the eye.5,11
Clinical signs and symptoms may include an often painless pulsatile exophthalmos, diplopia, strabismus, increased intraocular pressure (IOP), chemosis, orbital congestion, headache, perception of a rushing orbital sound on auscultation (ocular bruit), stasis retinopathy and central retinal vein occlusion in severe cases.5,11-13 The fistula may be idiopathic or a result of trauma.5 Imaging such as magnetic resonance angiography is indicated, and the patient should continue long-term care with ophthalmology.5 Treatment may include observation or endovascular surgical techniques with the aim of preserving the internal carotid artery.11
Episcleritis. In this condition, the superficial vascularized tissue between the conjunctiva and sclera—the episclera—becomes inflamed and mildly hyperemic in a localized area due to immune cell activation, release of inflammatory mediators, vasodilation and increased vascular permeability.1,2,14,15 Patients may be symptomatic for sectoral and interpalpebral redness, mild irritation and pain in cases of nodular episcleritis.2,14 This condition generally resolves in a self-limiting fashion within several hours to several days without intervention.14 In more symptomatic cases, treatment includes topical lubrication with artificial tears, oral NSAIDs, topical NSAIDs and topical steroids.1,2
Most cases of episcleritis are idiopathic, but further workup for systemic associations is warranted in recurrent or worsening cases.1 This condition is more common in females in the fifth decade of life and those with underlying autoimmune conditions.1,2 Episcleritis can be distinguished from scleritis by its response to topical 10% phenylephrine; in the former, redness dissipates after 10 to 15 minutes post-drop instillation due to vascular constriction, with maximum effect at one minute.1,2,14 Furthermore, the vasculature in episcleritis is mobile, while in scleritis the inflamed vessels do not move with a cotton-tipped applicator.2
Subconjunctival hemorrhage. This condition results from ruptured conjunctival blood vessels that lead to accumulation of blood beneath the conjunctiva.1,2,16 These hemorrhages are typically painless and do not involve vision loss.2 Although patients may present with a high level of concern due to the acute appearance of blood on the surface of their eye, patient education is essential to convey the benign nature of this condition. This condition is self-limiting, and full blood resorption is expected within a few weeks without intervention, although artificial tear use and warm compresses may help to ameliorate symptoms.1,2
Neurotrophic keratopathy. These patients develop reduced or absent corneal sensation with subsequent corneal epitheliopathy.17 They often present with ocular signs that are disproportionately worse than symptoms and, in many cases, may be asymptomatic.18 Patient-reported symptoms may include hyperemia and decreased vision, while a spectrum of clinical signs can be evident ranging from mild epithelial and tear film changes to severe corneal ulceration, stromal melting and/or perforation.17,19 Treatments vary based on severity and can include copious lubrication, topical anti-infective or anti-inflammatory agents, autologous serum tears, bandage contact lenses, amniotic membranes, punctal plugs, tarsorrhaphy and topical cenegermin drops.17,20
 |
| This patient has sectoral episcleritis. Click image to enlarge. |
Conditions With Moderate to Severe Pain
Other conditions—some more common than others—are associated with moderate to severe pain. These include anterior uveitis, scleritis, microbial keratitis, contact lens-induced acute red eye (CLARE), acute angle-closure glaucoma and photokeratitis, to name a few.
Anterior uveitis. Breakdown of the blood-aqueous barrier leads to inflammation of the uveal tract, including of the iris and/or ciliary body, and is known as anterior uveitis.2,21,22 Patients are typically symptomatic for moderate to severe ocular pain, redness, epiphora and photophobia, and signs include presence of cells and flare in the anterior chamber and a circum ciliary flush near the limbus.2 While first-time occurrences, particularly if unilateral, are typically idiopathic, certain systemic conditions and medications may underlie anterior uveitis and include spondyloarthropathies (with patients often testing positive for HLA-B27), infectious disease (e.g., syphilis, tuberculosis, Lyme, herpes virus) and use of sulfonamides, cidofovir and rifabutin.2,21
Treatment of anterior uveitis includes frequent instillation of topical ophthalmic steroids to address local ocular inflammation as well as topical cycloplegic agents to stabilize the permeability of leaky and inflamed iris vessels and paralyze the ciliary body to provide analgesia. A laboratory workup may be considered to elucidate underlying autoimmune or infectious etiologies, particularly in recurrent or bilateral and granulomatous cases.2,21
Scleritis. In anterior scleritis, scleral inflammation results in vascular engorgement of the deep episcleral plexus, which is also displaced outward by an edematous sclera.23 This leads to a characteristic blue-violet tinge to the sclera, redness that does not blanch with the installation of topical phenylephrine, severe and boring ocular pain, which is worse at night and with eye movements, and photophobia.2,14,24
Anterior scleritis can be diffuse, nodular or necrotizing. This condition is often associated with autoimmune and systemic diseases including rheumatoid arthritis and granulomatosis with polyangiitis, although infectious etiologies may also be possible.2,14 In the necrotizing form, peripheral ulcerative keratitis may be present marked by substantial amounts of peripheral subepithelial corneal infiltration.2 A common cause of this is Stevens-Johnson syndrome, which is often precipitated by recent oral penicillin antibiotic use. Topical cycloplegia and topical steroid use must be coupled with switching the oral antibiotic and systemic anti-inflammatory treatment to prevent scleral melting and globe perforation; close interdisciplinary care with a rheumatologist is essential.2,14
Microbial keratitis. Bacterial and fungal keratitis, also known as corneal ulcers, manifest as corneal epithelial defects that stain with sodium fluorescein overlying stromal infiltrates.2,25 Symptoms of microbial keratitis include photophobia, moderate to severe pain, conjunctival injection due to concurrent conjunctivitis, tearing and discharge.2,25 Its impact on vision is minimal if the ulcer is not within the visual axis. An anterior chamber reaction and hypopyon may also be noted, and severe cases may result in corneal perforation.2
Microbial keratitis is typically associated with predisposing risk factors, which include contact lens wear, ocular trauma, topical corticosteroid use, ocular surface disease, systemic diseases such as diabetes and agricultural work.2 Common causative organisms include Pseudomonas aeruginosa, Staphylococcus aureus and coagulase-negative staphylococci.2
Treatment consists of frequent instillation of fortified topical antibiotics and frequent ophthalmological follow-up.2 Clinical appearance of corneal infections may not always reliably predict the offending pathogen; therefore, specimen cultures may be obtained in order to help guide therapy.25
CLARE. Previously referred to as “contact lens overwear syndrome” or “immobile lens syndrome,” this is an inflammatory corneal infiltrative event generally associated with soft contact lens overwear.26 Symptoms generally include mild pain or irritation, moderate to severe hyperemia in a circumferential pattern due to concurrent conjunctivitis, tearing and photophobia.2 CLARE may consist of multiple small (less than 1mm in size) focal infiltrates or diffuse infiltration without corneal haze, generally found in the midperiphery or periphery of the cornea with minimal punctate staining overlying the infiltrates.26
The etiology of CLARE may be related to contact lens care solutions and cases contaminated with microbes, particularly in the setting of contact lens overwear, poor contact lens hygiene practices or tightly fitting lenses secondary to improper design or lens dehydration.27 Treatment includes temporary discontinuation of contact lens wear until complete resolution of signs and symptoms, copious ocular lubrication with preservative-free artificial tears and instillation of topical antibiotics with or without the use of topical ophthalmic steroids in more severe cases.28,29
Patient education is vital; wearing time should be decreased, overnight wear should be discontinued and contact lens hygiene should be stressed, with single-use daily contact lens wear modalities preferred.29 The fit should be reassessed before use begins again.
Acute angle-closure glaucoma. This occurs when the anterior chamber angle closes off and a subsequent elevation in IOP results in damage to the optic nerve.2 The acute IOP spike results in diffuse hyperemia and ciliary flush due to vascular congestion.30 Additional ocular symptoms include moderate to severe pain, photophobia, decreased vision, a mid-dilated and non-reactive pupil, a shallow anterior chamber angle and perception of halos around lights, along with headache, nausea and vomiting.2,30 Patients are at greater risk for acute angle-closure glaucoma if they are female, middle-aged, of Asian ethnicity, hyperopic with a shallow anterior chamber or are using certain medications such as topiramate or sulfas.2
Prompt treatment is imperative and includes compression gonioscopy, topical beta-blockers, topical brimonidine, topical and oral carbonic anhydrase inhibitors (including acetazolamide IV or oral) and timely pilocarpine, a parasympathomimetic, when IOP is reduced to 30mm Hg or less.2,30 Medications that can cause further dilation, such as apraclonidine, may be contraindicated.2 Once IOP stabilizes and the hazy cornea clears, a laser iridotomy is performed in order to facilitate aqueous drainage for the long term.2,30
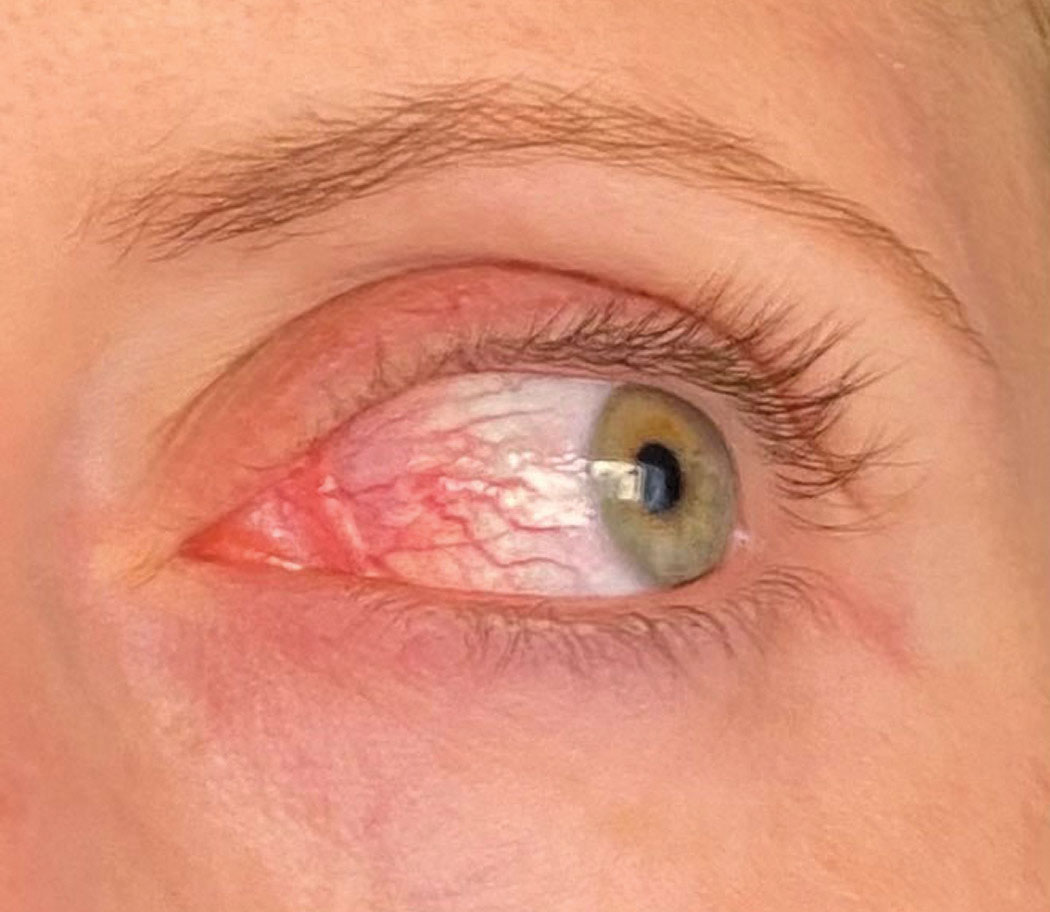 |
| Sectoral episcleritis from a different angle in the same patient in the previous photo. Click image to enlarge. |
Corneal abrasion and foreign body injury. Corneal abrasions result from breaks to the corneal epithelium and can lead to acute symptoms of moderate to severe pain, discomfort, tearing and photophobia, often resolving within 48 hours.2,31 Hyperemia occurs from conjunctival inflammation, and vision is affected if the corneal defect is central. Ocular foreign bodies may result in corneal abrasions if they disrupt the corneal epithelium; in particular, foreign bodies trapped under the eyelid may rub along the corneal surface and cause a linear defect.2,31
In cases of severe pain and discomfort, a topical anesthetic may be instilled to relieve pain and assist with the eye examination.1,2 Sodium fluorescein is instilled to assess the pattern and extent of the epithelial defect under a cobalt blue filter.1,2 When a foreign body is suspected, it is recommended to examine the superior palpebral conjunctiva with lid eversion in order to identify whether there is a retained foreign body under the upper lid so that it may be removed.1,2
Treatment of corneal abrasions, after the presence of foreign body has been ruled out, begins with topical antibiotics and may eventually involve the addition of topical lubrication, topical cycloplegics and topical NSAIDS. To resolve residual inflammation or the appearance of subepithelial corneal infiltrates later on, topical steroids may be added. Oral analgesics may also be considered for cases producing significant pain.1,2
Eye patching was previously an accepted mode of treatment for corneal abrasions but has since been outmoded following data demonstrated by a corneal abrasion pressure patch study.1,32 Many still prefer to patch larger abrasions; it reminds patients to remain sedentary during recovery, provides a level of analgesia and allows the corneal epithelium to be free from the risk of eye rubbing over the initial healing period. In severe cases, bandage contact lens wear or amniotic membranes may be considered. Follow-up should occur in 24 hours to ensure no secondary complications exist (microbial keratitis, the discovery of another foreign body, etc.).1,2
Photokeratitis. Ocular exposure to ultraviolet rays, because of the cornea’s propensity to absorb that wavelength of light, particularly UV-C, can lead to acute epithelial necrosis resulting in photokeratitis.33 Symptom onset typically occurs six to eight hours after UV exposure and results in severe bilateral pain, photophobia, epiphora, foreign body and blepharospasm.33,34 Hyperemia will also be present. This condition is more common in patients with occupational exposure, such as welding without adequate eye protection, or patients who are exposed to excessive sunlight in the mountains, particularly on a bright, snowy day.5,34 Photokeratitis is self-limiting, as the corneal epithelium typically regenerates within 48 hours; however, oral analgesics and topical ophthalmic antibiotic/steroid ointments along with cycloplegia can be used to protect the ocular surface from infection and provide symptom relief.5,34 In cases where there is significant corneal edema, hypertonic drops and ointments can be added.
Chemical burns to the ocular surface. This can result in significant vision loss within a short period of time.35 Symptoms can vary from mild ocular irritation to severe damage of the anterior ocular structures with corneal opacification.35 Ocular burns from acidic agents tend to be less severe than from alkali agents, although the latter tend to be more common due to their ubiquitous availability in products such as cleaning agents. Emergent treatment is indicated in the setting of an acute ocular burn and includes copious lubrication, such as with a Morgan lens, with intermittent pH assessment, as well as topical steroid, topical antibiotic and topical and oral ascorbate use (vitamin C).33,35 Additional treatments may include autologous serum tears, bandage contact lenses, amniotic membranes, oral tetracyclines, cycloplegia, tenoplasty, debridement of necrotic tissue, tectonic keratoplasty, tissue adhesives and limbal stem cell transplantation in severe cases.30,36
Graft rejection. When corneal health is compromised or irregularities preclude useful vision, corneal transplantation (keratoplasty) may be necessary, in which the host is surgically grafted with donor tissue.37 As with any transplantation surgery, several risks are involved, including the host’s immunological rejection of the donor corneal tissue, which may occur in any corneal layer at any point after keratoplasty and may lead to graft failure.37,38 Patients may be symptomatic for redness, photophobia, pain, epiphora and/or decreased vision, while clinical signs of immunological rejection include corneal edema, vascularization, keratic precipitates, subepithelial or stromal infiltrates, a Khodadoust line or an epithelial rejection line.39
Treatment of graft rejection involves the use of topical immunosuppressants such as steroids, which are generally also used in the long term to prevent rejection episodes. Systemic immunosuppressants may be considered in high-risk grafts.40
Conjunctivitis and keratitis with visual manifestations. While most cases of infectious conjunctivitis generally involve minimal pain and vision loss, gonococcal (bacterial) conjunctivitis and EKC (viral) are exceptions. These conditions may present with acute presentations of conjunctivitis involving copious discharge, hyperemia and vision loss.41,42 Similarly, while microbial keratitis can often spare vision when the ulcer is non-central, ulceration within the visual axis can lead to marked vision loss.2,25
 |
| Sectoral episcleritis is evident in this eye. Click image to enlarge. |
Endophthalmitis. This is a microbial infection of the aqueous and vitreous humor.2,43 This condition results in symptoms of moderate to severe pain, photophobia, decreased vision, eyelid edema and ocular discharge, and signs may include a hypopyon, iris synechiae, fibrinous membranes in the anterior chamber and vitreal inflammation.2,11,44 Significant conjunctival hyperemia may be seen due to conjunctivitis and circum-corneal congestion.44 Infection is often exogenous and can occur about 12 hours to seven days after penetrating ocular surgery, trauma or injections, as well as from severe corneal infections, hospitalization with IV, parenteral nutrition or broad-spectrum antibiotic use.2,43 Emergent referral to ophthalmology is warranted, and treatment may consist of intravitreal antimicrobial injections or vitrectomy, with varied visual outcomes.2,43
Takeaways
While patients will often present with a subjective complaint of red eyes, the underlying etiologies are numerous, and an accurate history and clinical examination are vital for appropriate care. Taking a systematic approach to the exam is imperative and will in many cases lead to the correct diagnosis or a narrower list of differentials.
Dr. Sherman is an assistant professor and director of optometric sciences at Columbia University Irving Medical Center. She specializes in complex and medically necessary contact lens fittings, anterior segment disease and primary care. Dr. Cherny is a resident at the Massachusetts Eye and Ear Infirmary, where she is focusing on cornea and specialty contact lenses, as well as ocular disease and emergency eye care. She graduated from the SUNY College of Optometry with a micro-credential in advanced cornea and contact lenses. Neither author has any financial interests to disclose.
1. Cronau H, Kankanala RR, Mauger T. Diagnosis and management of red eye in primary care. Am Fam Physician. 2010;81(2):137-44. 2. Gilani CJ, Yang A, Yonkers M, et al. Differentiating urgent and emergent causes of acute red eye for the emergency physician. West J Emerg Med. 2017;18(3):509-17. 3. Høvding G. Acute bacterial conjunctivitis. Acta Ophthalmol. 2008;86(1):5-17. 4. Ryder EC, Benson S. Conjunctivitis. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021. 5. Frings A, Geerling G, Schargus M. Red eye: a guide for non-specialists. Dtsch Arztebl Int. 2017;114(17):302-12. 6. Najmi H, Mobarki Y, Mania K, et al. The correlation between keratoconus and eye rubbing: a review. Int J Ophthalmol. 2019;12(11):1775-81. 7. Messmer EM. The pathophysiology, diagnosis, and treatment of dry eye disease. Dtsch Arztebl Int. 2015;112(5):71-82. 8. Bernardes TF, Bonfioli AA. Blepharitis. Semin Ophthalmol. 2010;25(3):79-83. 9. Rouen PA, White ML. Dry eye disease: prevalence, assessment, and management. Home Healthc Now. 2018;36(2):74-83. 10. Golden MI, Meyer JJ, Patel BC. Dry Eye Syndrome. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021. 11. Henderson AD, Miller NR. Carotid-cavernous fistula: current concepts in aetiology, investigation, and management. Eye (Lond). 2018;32(2):164-72. 12. Lau FH, Yuen HK, Rao SK, Lam DS. Spontaneous carotid cavernous fistula in a pediatric patient: case report and review of literature. J AAPOS. 2005;9(3):292-4. 13. Kochar B, Shan SJ, Anand G, et al. Totally one-sided: painless unilateral proptosis. Am J Med. 2015;128(4):361-3. 14. Héron E, Bourcier T. Scleritis and episcleritis. J Fr Ophtalmol. 2017;40(8):681-95. 15. Schonberg S, Stokkermans TJ. Episcleritis. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021. 16. Sahinoglu-Keskek N, Cevher S, Ergin A. Analysis of subconjunctival hemorrhage. Pak J Med Sci. 2013;29(1):132-4. 17. Dua HS, Said DG, Messmer EM, et al. Neurotrophic keratopathy. Prog Retin Eye Res. 2018;66:107-31. 18. Mantelli F, Nardella C, Tiberi E, et al. Congenital corneal anesthesia and neurotrophic keratitis: diagnosis and management. Biomed Res Int. 2015;2015:805876. 19. Rama P, Sacchetti M. Neurotrophic keratopathy. Orphanet. March 2017. www.orpha.net/consor/cgi-bin/OC_Exp.php?lng=EN&Expert=137596. Accessed Septemer 10, 2021. 20. Sheha H, Tighe S, Hashem O, et al. Update on cenegermin eye drops in the treatment of neurotrophic keratitis. Clin Ophthalmol. 2019;13:1973-80. 21. Gueudry J, Muraine M. Anterior uveitis. J Fr Ophtalmol. 2018;41(1):e11-21. 22. Duplechain A, Conrady CD, Patel BC, et al. Uveitis. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021. 23. Krachmer J, Mannis M, Holland E. Cornea, 2nd ed. Elsevier Mosby; 2005, 1284-314. 24. Okhravi N, Odufuwa B, McCluskey P, et al. Scleritis. Surv Ophthalmol. 2005;50(4):351-63. 25. Farahani M, Patel R, Dwarakanathan S. Infectious corneal ulcers. Dis Mon. 2017;63(2):33-7. 26. Efron N, Morgan PB. Can subtypes of contact lens-associated corneal infiltrative events be clinically differentiated? Cornea. 2006;25(5):540-4. 27. Khan SA, Lee CS. Recent progress and strategies to develop antimicrobial contact lenses and lens cases for different types of microbial keratitis. Acta Biomater. 2020;113:101-18. 28. Holden BA, La Hood D, Grant T, et al. Gram-negative bacteria can induce contact lens related acute red eye (CLARE) responses. CLAO J. 1996;22(1):47-52. 29. Shovlin J. Clear cause of CLARE. Rev Optom. 2004;141(9). 30. Pohl H, Tarnutzer AA. Acute angle-closure glaucoma. N Engl J Med. 2018;378(10):e14. 31. Ahmed F, House RJ, Feldman BH. Corneal abrasions and corneal foreign bodies. Prim Care. 2015;42(3):363-75. 32. Turner A, Rabiu M. Patching for corneal abrasion. Cochrane Database Syst Rev. 2006;(2):CD004764. 33. Sharma N, Kaur M, Agarwal T, et al. Treatment of acute ocular chemical burns. Surv Ophthalmol. 2018;63(2):214-35. 34. Cullen AP. Photokeratitis and other phototoxic effects on the cornea and conjunctiva. Int J Toxicol. 2002;21(6):455-64. 35. Adepoju FG, Adeboye A, Adigun IA. Chemical eye injuries: presentation and management difficulties. Ann Afr Med. 2007;6(1):7-11. 36. Baradaran-Rafii A, Eslani M, Haq Z, et al. Current and upcoming therapies for ocular surface chemical injuries. Ocul Surf. 2017;15(1):48-64. 37. Akanda ZZ, Naeem A, Russell E, et al. Graft rejection rate and graft failure rate of penetrating keratoplasty (PKP) vs lamellar procedures: a systematic review. PLoS One. 2015;10(3):e0119934. 38. Velásquez-Monzón K, Navarro-Peña MC, Klunder-Klunder M, et al. Pediatric penetrating keratoplasty and graft rejection: experience at the Hospital Infantil de México Federico Gómez. Bol Med Hosp Infant Mex. 2020;77(1):23-7. 39. Anderson, E, Chang V, Bunya V, et al. Corneal allograft rejection and failure. AAO Eyewiki. April 12, 2021. eyewiki.aao.org/Corneal_Allograft_Rejection_and_Failure#Definition_of_graft_rejection_vs_failure. Accessed September 6, 2021. 40. Di Zazzo A, Kheirkhah A, Abud TB, et al. Management of high-risk corneal transplantation. Surv Ophthalmol. 2017;62(6):816-27. 41. Wegman DH, Guinee VF, Milian SJ. Epidemic keratoconjunctivitis. Am J Public Health Nations Health. 1970;60(7):1230-7. 42. Belga S, Gratrix J, Smyczek P, et al. Gonococcal conjunctivitis in adults: case report and retrospective review of cases in Alberta, Canada, 2000-2016. Sex Transm Dis. 2019;46(1):47-51. 43. Durand ML. Endophthalmitis. Clin Microbiol Infect. 2013;19(3):227-34. 44. Simakurthy S, Tripathy K. Endophthalmitis. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021. |
