Pathways to Premium IOL Outcomes & Successful
Surgical Comanagement
How the right approach to pre- and postoperative care can ensure optimal IOL outcomes for your patients.Sponsored by Johnson & Johnson VisionBy Marc Bloomenstein OD, FAAO; Paul M. Karpecki, OD, FAAO; Amy Nau, OD, OD
Release Date:June 15, 2019
Expiration Date:
June 30, 2020
Goal Statement:
Upon completing this educational activity, optometrists should have improved the skills to evaluate the right patients for potential premium IOL technology, address ocular surface issues in advance of procedures, comanage patients with the surgical center, and offer optimal care to patients pre- and postoperatively.
Faculty/Editorial Board:
Marc Bloomenstein OD, FAAO; Paul M. Karpecki, OD, FAAO; Amy Nau, OD, OD
Credit Statement:
This course is COPE approved for 2 hours of CE credit. COPE ID is 62523-PO. Please check your state licensing board to see if this approval counts toward your CE requirement for relicensure.
Joint-Sponsorship Statement:
This continuing education course is joint sponsored by the University of Alabama School of Optometry.
Disclosure Statement:
Dr. Karpecki is a consultant for Aerie Pharmaceuticals, Abbott Medical Optics, Akorn, Alcon, Allergan, Anthem, Avellino Labs, Bausch + Lomb, Beaver-Visitec, Bio-Tissue, BlephEx, Bruder Healthcare, Cambium Pharmaceuticals, Calhoun Vision/Rx Sight, Essilor, eyeBrain, Eye Gate Medical, Eyemaginations/Rendia, Eyes4Lives, Focus Labs, iCare USA, Imprimis Pharmaceuticals, Katena, Konan Medical, Lubris Inc., MacuLogix, Oasis Medical, Ocular Therapeutix, Oculus, OcuSoft, Paragon Biotek, PECAA, Perrigo, Quark Pharmaceuticals, Regeneron, Reichert/Ametek, Retina Sciences, Science Based Health, SightRisk, Shire Pharmaceuticals, TearFilm Innovations, TearLab, TearScience, TelScreen, Topcon, Visiometrics, Vision Care Inc. and Vmax; and a research grant principal investigator for Shire Pharmaceuticals; has received honoraria for the speaker’s bureau of Glaukos; is a stockholder in Eye Therapies; is on the board of Optometric Medical Solutions, Bruder Healthcare and TearLab.
Dr. Bloomenstein is a consultant for OcuSoft and Reichert; is a stock shareholder in TearLab; and is on the speaker’s bureau of Allergan, Bausch + Lomb and Alcon.
Dr. Nau is on the speaker’s bureau of Johnson & Johnson Vision.
Supported by: An unrestricted educational grant from Johnson & Johnson Vision.
Correcting Presbyopia Using Innovative IOL Technology
By Marc Bloomenstein, OD, FAAO
 |
Patient lifestyles and evolving technology are transforming the way we treat the growing population of presbyopic patients. Today’s presbyopes live their lives differently than previous generations. They are more active, they are working longer, and their near vision is defined as the ability to view cell phones and other digital devices clearly. Moreover, they want to look younger and be free from the burden of eyeglasses.
We need to keep in mind that today’s presbyopia patients have higher expectations regarding presbyopia correction, so traditional options most likely will fall short.
Discussing Presbyopia With Patients
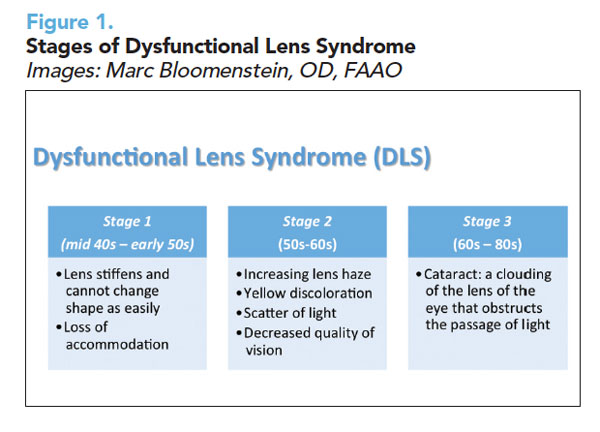
We play an important role in educating our patients about the visual changes that occur as they age. The term dysfunctional lens syndrome (DLS)—which describes the natural changes that occur in the crystalline lens after about age 42—is a good way to explain this natural process to patients. We should begin the conversation about DLS when patients are in their 30s and 40s.
Wrinkles, gray hair, and other changes occur as we age, and the crystalline lens is not immune to the aging process. Over time, layers are added to the lens, which become more compact. In addition, disulfide bonds accumulate, and the lens stiffens, leading to changes in optics. Diagnostic technology can help us evaluate how patients’ vision quality is declining.
Figure 1 shows DLS stages.
In stage 1, we can prescribe reading glasses, multifocal contact lenses, corneal inlays, or blended or monovision laser vision correction or offer refractive lens exchange.
In stage 2, we need to talk to patients about subjective symptoms, knowing that lenticular changes will affect their vision even in the absence of a refractive change. Therefore, we should reassure patients that we will continue monitoring their eyes and ask them to notify us of vision changes.
In stage 2, presbyopia can be treated with reading glasses or multifocal contact lenses, as well as the surgical opportunities of stage 1 DLS.
In stage 3, cataract surgery becomes necessary, with monofocal intraocular lenses (IOLs) (distance or monovision) or presbyopia-correcting IOLs.
 | |
|
When our patients have cataract surgery, we should be providing preoperative care, referrals, and postoperative care. As optometrists, we should select surgeons whose philosophies match our own and forge a strong relationship them. We need to share relevant information with them about the patients they will treat, and we need to talk to patients about what to expect when they see the surgeon.
Presbyopia-Correction Options
Each presbyopia-correction option has advantages and disadvantages. For example, studies have shown that progressive lenses can contribute to falls, while patients often dislike the interference of reading glasses. Presbyopic contact lenses can be challenging because of comfort issues in older eyes, visual acuity problems, and chair time for the practitioner, although advances have been made to remedy some of these limitations. With regard to IOL options, here are some observations:
 |
| Click image to enlarge. |
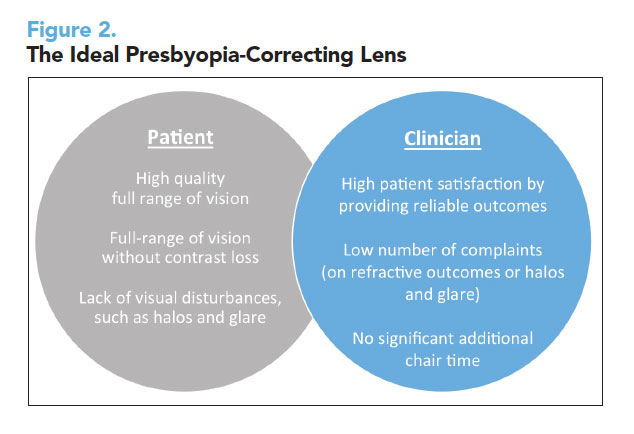
Presbyopia-correcting or lifestyle IOLs, as I refer to them, appeal to patients who desire spectacle independence for near vision (Figure 2).
Monofocal monovision provides monofocal quality of vision, and many patients have been satisfied with this option.1 However, some patients have reported reduced depth perception, a feeling of imbalance, and limited intermediate vision. And patients still need to use glasses for night driving and prolonged reading. Monovision with an IOL is not the same as the contact lens version because the lens always adds some accommodative effect, although small.
In recent years, multifocal technology has advanced.2 Low-add multifocal IOLs provide near and distance vision, although intermediate vision may be limited. Patients may also have dysphotopsia and need to neuroadapt to the lenses.
Extended depth of focus (EDOF) IOLs are diffractive lenses that extend vision instead of offering discrete close, intermediate, or distance vision. The extension of the focal range means there is more than one sweet spot.3 Patients are more tolerant of unexpected residual refractive error, which is also helpful as a patient’s ocular surface changes with age.4 Patients have a full range of high-quality continuous vision with a low incidence of visual symptoms and require glasses less often. I find that patients only need a slight magnification for very small print. We have obtained good results with this lens in patients with macular degeneration or previous refractive surgery. Approximately 85% of patients with EDOF IOLs wear glasses sometimes.5
Personalized Vision
Surgeons can personalize patients’ vision with mini-monovision, or mix and match within a platform of presbyopia-correcting IOLs. In our practice, we implant the EDOF IOL in the dominant eye. If patients cannot read as well as they would like, we personalize their nondominant eye with a low-add multifocal IOL.6 If patients are pleased with their vision in the first eye, we implant the EDOF lens in the other eye. Mixing and matching presbyopic IOLs offers an increased range of vision and improves patients’ near vision.
Making a Match
When matching presbyopia-correction technology with the appropriate patient, questionnaires can help us learn more about our patients. We need to know patients’ preferred reading distance, their leisure pursuits and career demands, and how they rate near, intermediate, and distance in terms of importance. I give patients the near point card upside down and then I drop it on the floor. When they pick it up, they automatically adjust it to where they want to read and we can see their natural reading position.
We cannot underestimate the importance of optimizing intermediate distance. Patients spend the vast majority of their time using distance and intermediate vision—looking at the dashboard, driving, using a computer, and watching television.
In our practice, we do not offer patients a range of options. We write down the option that best fits their needs and desires. In fact, patients are not looking for choices; they are looking for the solution that will provide the vision they need.
We need to manage patients’ expectations before surgery, discussing their postoperative vision and healing, as well as the potential need for glasses for small print and the possibility of glare and halos during adaptation. In addition, we must inform them that postoperative enhancement occasionally is needed.
It is especially important to manage expectations in myopic patients. These patients should recognize that monofocal IOLs will permanently give them distance vision.
During preoperative visits, optometrists need to prepare patients for the choices they will make when they see the surgeon. It helps to provide information on your website or give patients information to bring home. We also need to examine and treat the ocular surface well ahead of the time for referral. In fact, ocular surface treatment should start at stage 1 DLS.
Postoperative Care
When examining patients after cataract surgery with presbyopic IOLs, it’s important to check their binocular uncorrected vision. We should remind patients of restrictions and that they initially may feel off balance, but by emphasizing their binocular vision, we can reinforce that they use both eyes.
One week after surgery, ask patients how they are feeling and examine them, looking for signs of infection or increased inflammation. One month after surgery, make sure to examine patients again and check how they are functioning. During postoperative visits, we remind them that it will take time to neuroadapt to the new lens. I cannot emphasize enough that patients expect the optometrist to let them know how they are doing.
If results are not as expected, I learned an easy way to remember what to search for from a renowned surgeon, Eric Donnenfeld, MD. Dr. Donnenfeld recommends looking at the five “C”s—check the corneal surface, the capsule (and do a glare test), cystoid macular edema, correction, and centration. By evaluating the five “C”s, you almost always find a reason for results that are less than perfect.
After each examination, results should be sent to the surgeon.
Making the Choice Early
Our patients are living longer, working longer, and are active. The notion of optimizing reading vision is one that becomes more interpretative. The route patients choose to correct presbyopia will impact their daily lives, and we can help them navigate this journey earlier rather than later.
| 1. Ito M, Shimizu K, Iida Y, Amano R. Five-year clinical study of patients with pseudophakic monovision. J Cataract Refract Surg. 2012; 38:1440–1445. 2. Kim JS, Jung JW, Lee JM, et al. Clinical outcomes following implantation of diffractive multifocal intraocular lenses with varying add powers. Am J Ophthalmol. 2015; 160:702–709. 3. Cochener B. Tecnis Symfony intraocular lens with a “sweet spot” for tolerance to postoperative residual refractive errors. Open J Ophthalmol. 2017; 7:14–20. 4. Carones F. Residual astigmatism threshold and patient satisfaction with bifocal, trifocal and extended range of vision intraocular lenses (IOLs). Open J Ophthalmol. 2017; 7:1–7. 5. TECNIS Symfony® Extended Range of Vision IOLs DFU. Santa Ana, Calif. Johnson & Johnson Surgical Vision, Inc. 6. Black S. A clinical assessment of visual performance of combining the TECNIS® Symfony Extended Range of Vision IOL (ZXR00) with the +3.25 D TECNIS Multifocal 1-piece IOL (ZLB00) in subjects undergoing bilateral cataract extraction. Clin Ophthalmol. 2018; 12:2129–2136. 1. |
Marc Bloomenstein, OD, FAAO, practices with the Schwartz Laser Eye Center in Scottsdale, Ariz.
Managing Astigmatism Using Innovative IOL Technology
By Paul M. Karpecki, OD, FAAO
 |
To help patients achieve good uncorrected vision from cataract surgery, it is critical to correct astigmatism; this will greatly improve vision at all distances.
And while more than 50% of patients with astigmatism are eligible for correction with a toric intraocular lens (IOL), only 20% of patients with clinically significant astigmatism receive these lenses, according to the 2018 ASCRS Clinical Survey.1-3
In my experience, one reason patients do not have their astigmatism treated during cataract surgery is because they are not aware this option is possible. As the eyecare practitioners who spend the most time with patients, optometrists are in a key position to educate them about astigmatism and recommend solutions.
Preoperative Diagnostics
Keratometry or an autorefraction is usually adequate when assessing astigmatism power and axis preoperatively in most toric IOL candidates. Optical biometry, corneal topography, and optical coherence tomography are also useful tools for preoperative assessments. If astigmatism is present on the posterior surface of the cornea, it will appear on the Ks.4
During the preoperative examination, keratometry values should be compared with cylinder in the manifest refraction. If a discrepancy is identified, consider other causes of cylinder, such as lenticular astigmatism or dry eye disease. We can also assess patients’ refractive stability by monitoring the manifest refraction.
When evaluating data from assessments, consistency is critical. If readings are inconsistent, assessments should be repeated. We also need to compare previous measurements to determine stability. Axis measurements should be within 10 degrees, and magnitude measurements should be within 0.5D of previous readings. Keratometry readings should be within 1.0D of the fellow eye.
Measurements also should be repeated if there is high astigmatism in either eye (2.50D or greater) or the patient has small or large eyes (corneal diameter less than 10.75mm or greater than 13.0mm), or steep or flat eyes (40.0D or less or greater than 47.0D).
The most frequent reason for inconsistency is ocular surface disease. We need to be sure the patient has a healthy tear film before performing preoperative measurements.5 If topography shows signs of ocular surface disease, evaluate and treat the tear film before repeating measurements. To reduce error, it is also important to use the same device before and after surgery, use select technicians, and perform measurements before eyedrops are instilled.
Correcting Astigmatism
There are several alternatives when performing cataract surgery in patients with astigmatism—monofocal IOLs with incisional correction (via on-axis incision, or corneal relaxing incisions with a blade or femtosecond laser) for patients with less than 1.0D of astigmatism and toric IOLs (e.g., monofocal, extended depth of focus, multifocal, and pseudo-accommodating).
The goals of implanting toric IOLs are to deliver excellent visual acuity, reduce or eliminate astigmatic error, and achieve patient satisfaction. In a meta-analysis, Kessel et al. determined that postoperative corrected distance vision and spectacle independence for distance were better in patients who received toric IOLs versus those who had non-toric IOLs, with or without relaxing incisions.6 Black reported that 94% of eyes achieved 0.50D or less residual refractive error after implantation of toric IOLs.7
Toric IOLs are placed closest to the nodal point, so patients have very little distortion or rotation. These IOLs yield better vision than patients can achieve with glasses or contact lenses. That said, patients with high levels of astigmatism have a slight amount of peripheral distortion with toric IOLs, but still not as much as with glasses.
Patient Selection
The right presbyopic toric IOL candidates should want good uncorrected distance vision without glasses, but be comfortable with glasses for near. It is important to rule out significant or unstable corneal disease affecting the ocular surface or shape.
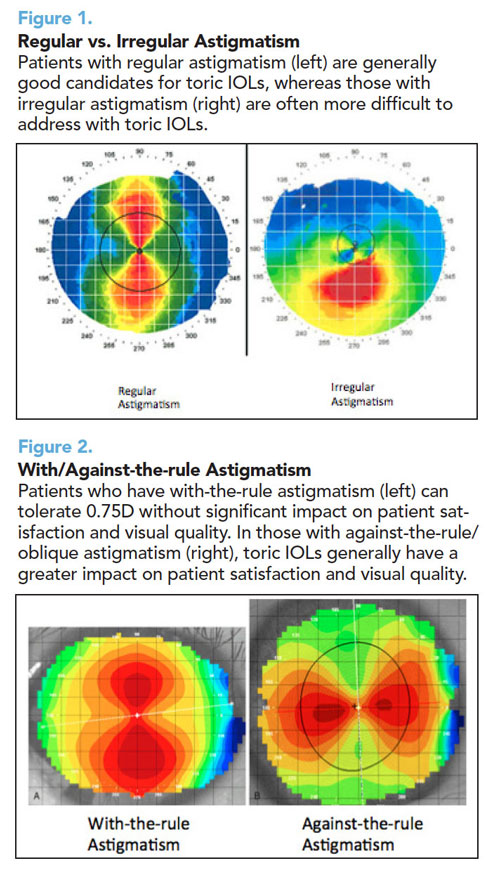 |
| Click on image to enlarge. |
In general, patients with more than 0.5D of regular astigmatism are good candidates for toric IOLs (Figure 1). Among patients who have with-the-rule astigmatism, those with 0.75D or more cylinder are good candidates (Figure 2). However, it is important to determine that the astigmatism is corneal astigmatism, using corneal topography or keratometry (not the refraction). If astigmatism is in the lens, it will be corrected when the cataract is extracted.
If a patient has against-the-rule or oblique astigmatism, correcting 0.5D of astigmatism will significantly improve vision.
Impact of Residual Astigmatism
The most likely cause of patient dissatisfaction with toric IOLs is postoperative residual astigmatism, according to anecdotal reports. In addition, one study reported that if more than 1% of rotation occurred, it decreased the effect of the toric IOL by 3.3%; with 10% rotation, patients lost 33% of the effect.8
Patients receiving presbyopia-correcting IOLs have very high expectations of their visual outcomes. Although monofocal IOL patients previously tolerated astigmatism, toric presbyopic IOL patients have paid to reduce their dependence on glasses, so they have less tolerance for astigmatism.
Managing Residual Astigmatism
If patients have residual astigmatism after implantation of a toric IOL, begin by looking at the manifest refraction. It should be repeated multiple times to determine whether it is stable before making a treatment decision.
We also need to examine the ocular surface. If significant ocular surface disease is present, it should be treated and then the manifest refraction repeated. In addition, we need to be sure the toric IOL is aligned properly.
There are several options to correct residual refractive error: glasses or contact lenses, limbal relaxing incisions or arcuate incisions, LASIK or PRK, IOL rotation, or IOL exchange.
Glasses or contact lenses are the easiest choice, but glasses may result in ghosting if the patient has significant astigmatism. Standard rigid gas permeable contact lenses unmask lenticular astigmatism, and corrected distance visual acuity may be suboptimal with toric rigid gas permeable lenses.
Limbal relaxing and arcuate incisions are low risk and relatively reliable. They can be made at the slit lamp. Make sure to treat refractive cylinder.
Toric IOL rotation may be considered in a dissatisfied patient in whom the IOL is off axis. This may occur if the target axis was incorrect, and there is a larger impact with higher toric corrections. The patient should have no significant spherical error, and the posterior capsule should be intact.
If there was an error in the spherical and cylindrical target, the IOL may be exchanged. We must first determine that astigmatism is regular or if spherical error is significant. If it is still early and the bag is intact, the surgeon can exchange the toric IOL. If not, a monofocal IOL should be considered. An exchange is dangerous if the capsule is open.
Note that IOL rotation or exchange should be done before a YAG procedure. It is also important to check for cystoid macular edema or other possible causes of decreased vision. If there is residual astigmatism, delay surgery on the second eye.
Educating Patients Early On
Growing numbers of patients will need cataract surgery in the future. To achieve optimal outcomes, astigmatism must be corrected. Optometrists play an important role in educating patients about astigmatism correction options during surgery and providing preoperative and postoperative care.
| 1. East Valley Ophthalmology website. Distribution of corneal astigmatism in normal adult population. Keratometry database. https://www.doctor-hill.com/iol-main/astigmatism_chart.htm Accessed April 1, 2019. 2. AcrySof® IQ Toric [product information]. Fort Worth, TX: Alcon Laboratories, Inc; 2009. 3. ASCRS 2018 Clinical Survey. http://supplements.eyeworld.org/eyeworld-supplements/december-2018-clinical-survey 4. Koch DD, Ali SF, Weikert MP, et al. Contribution of posterior corneal astigmatism to total corneal astigmatism. J Cataract Refract Surg. 2012; 38:2080–2087. 5. Epitropoulos AT, Matossian C, Berdy GJ, et al. Effect of tear osmolarity on repeatability of keratometry for cataract surgery planning. J Cataract Refract Surg. 2015; 41:1672–1677. 6. Kessel L, Andresen J, Tendal B, et al. Toric intraocular lenses in the correction of astigmatism during cataract surgery: a systematic review and meta-analysis. Ophthalmology. 2016; 123:275–286. 7. Black D. Efficacy of hydrophobic acrylic toric IOL to correct astigmatism in cataract patients. Presented at ASCRS 2015. 8. Bauer NJ, de Vries NE, Webers CA, et al. Astigmatism management in cataract surgery with the AcrySof toric intraocular lens. J Cataract Refract Surg. 2008; 34:1483-1488. 1. |
Dr. Karpecki is director of Corneal Services, the Advanced Ocular Surface Disease Center and Research at Kentucky Eye Institute in Lexington, Kentucky, and practices in the ocular surface disease clinic at Gaddie Eye Centers, Louisville, Ky.
Optimizing the Ocular Surface with Advanced Therapies
By Amy Nau, OD, FAAO
 |
It is our responsibility to address ocular surface disease (OSD) as part of preventative care. However, if patients are not in acute distress, noncompliance with recommendations is common. If we anticipate that a patient will require lid surgery, ocular surgery, or ocular injections, we must have a frank discussion about the importance of treating OSD to optimize surgical outcomes. In this context, patients are often much more adherent to therapy and continue treatment indefinitely.
Targeting OSD
Contemporary practice offers a wide range of options to treat OSD. Success is achievable when the root cause of the condition is identified and treated with the appropriate combination of targeted therapies.
The most common cause of OSD is meibomian gland dysfunction (MGD); thus, a thorough evaluation of the lids and lashes is a mandatory first step. Additional testing for lacrimal gland function, allergies, poor nocturnal lid seal, and neuropathic pain using a proparacaine challenge also should be included.
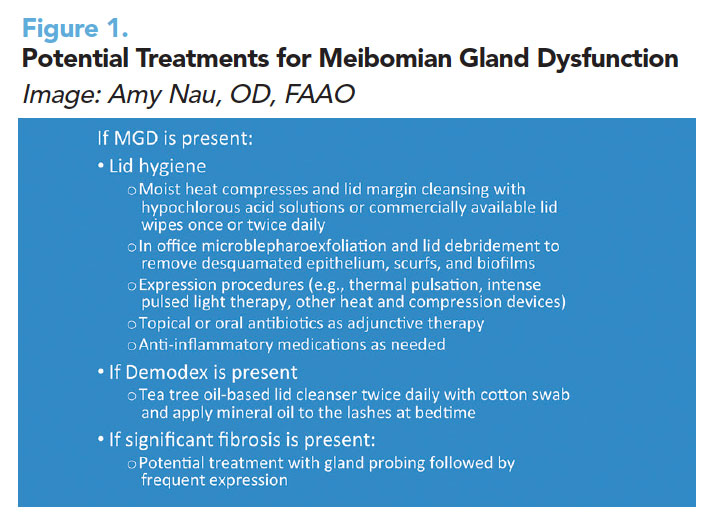
MGD is extremely common, but it is easy to overlook if we do not pay specific attention to the structure and function of the meibomian glands. Figure 1 shows potential treatments for MGD. Omega-3 fatty acid supplements often are used to treat OSD, but research varies on their effectiveness.1
 |
| Click image to enlarge. |
When patients have symptoms of dryness in the morning, we use the Korb-Blackie light test to determine if there is a poor nocturnal lid seal.2 In such cases, ointment before bedtime and/or a sleep mask will help alleviate symptoms and reduce inflammation by preventing overnight desiccating stress.
If patients’ MMP-9 results are positive, and they have a high tear osmolarity level or chronically injected red eyes, I prescribe a pulse dose of topical corticosteroids for two to four weeks.3 Non-preserved steroids have been shown to be more effective but need to be compounded.4 If patients have adhered to our recommendations and show limited improvement, and MMP-9 results are still positive at 10 to 12 weeks, I consider cyclosporine A drops or lifitegrast. If inflammation and symptoms persist after six months, autologous serum drops or amniotic fluid drops are good add-on medications. Compounded testosterone drops help with MGD and aqueous dry eye. Punctal plugs are effective, but contraindicated when inflammation is present. For patients with low tear volumes, nasal neurostimulation and hydroxypropyl cellulose ophthalmic inserts can help, but moisture chamber glasses and scleral lenses will help increase tear volumes by mechanical means. Amniotic membrane bandage lenses improve persistent corneal defects and reduce inflammation, but will not treat underlying conditions.
Patient Education and Involvement
It is very important for patients to understand their condition. In cases of MGD, we invoke a dental model, showing them their lids and explaining that the condition is similar to gingivitis, requiring ongoing hygiene and care. Showing them pictures and spending time reviewing their specific condition will enhance compliance. Patients need to understand that it often will take time for improvement, dry eye is often chronic, and lifestyle modifications such as reduced screen time and environmental changes are necessary. Our staff members play a vital role in reinforcing our treatment philosophy and providing very specific instructions.
| 1. Dry Eye Assessment and Management Study Research Group, et al. n-3 fatty acid supplementation for the treatment of dry eye disease. N Engl J Med. 2018; 378:1681–1690. 2. Korb D, Blackie C. The Korb-Blackie lid light test. Invest Ophthalmol Vis Sci. 2013;54:942. 3. Avunduk AM, Avunduk MC, Varnell ED, et al. The comparison of efficacies of topical corticosteroids and nonsteroidal anti-inflammatory drops on dry eye patients: a clinical and immunocytochemical study. Am J Ophthalmol. 2003; 136:593–602. 4. Hong S, Kim T, Chung SH, et al. Recurrence after topical nonpreserved methylprednisolone therapy for keratoconjunctivitis sicca in Sjögren’s syndrome. J Ocul Pharmacol Ther. 2007; 23:78–82. 1. |
Amy Nau, OD, FAAO, is managing partner with Korb and Associates in Boston, a practice focusing on dry eye and medical contact lenses.
